Dialectical Behaviour Therapy (DBT) is a form of psychotherapy that was developed by psychologist Marsha M. Linehan in the late 1980s. Originally designed to help individuals with borderline personality disorder, DBT has since been expanded to treat a range of mental health conditions, including depression, anxiety, eating disorders, and substance abuse.
DBT is based on the concept of dialectics, which refers to the integration of opposing ideas or perspectives. This approach emphasizes the need for balance between acceptance and change, and recognizes that individuals can hold contradictory thoughts and feelings. By helping individuals identify and resolve these conflicts, DBT aims to improve emotional regulation, interpersonal effectiveness, and overall well-being.
One of the key components of DBT is its focus on skills training. DBT teaches individuals a set of skills that can be used to effectively manage emotions, handle stressful situations, and improve interpersonal relationships. These skills include mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. By learning and practicing these skills, individuals can develop healthier coping mechanisms and more fulfilling relationships.
Another important aspect of DBT is the therapeutic relationship. DBT therapists provide a supportive and validating environment for their clients, while also challenging them to make positive changes. Through individual therapy sessions, group therapy, and phone coaching, therapists help individuals apply their skills in real-life situations and work towards their treatment goals.
In this comprehensive guide to Dialectical Behaviour Therapy, we will explore the key principles and techniques behind this therapeutic approach. Whether you are someone seeking therapy or a mental health professional looking to expand your knowledge, this guide will provide you with everything you need to know about DBT and how it can help individuals lead healthier and more fulfilling lives.
Understanding Dialectical Behaviour Therapy
Dialectical Behaviour Therapy (DBT) is a type of psychotherapy that was originally developed to treat borderline personality disorder (BPD). However, it has since been adapted to help individuals with a range of mental health conditions, including depression, anxiety, and substance abuse disorders. DBT combines elements of cognitive-behavioural therapy (CBT) with concepts from Buddhist philosophy, such as mindfulness and acceptance.
One of the main principles of DBT is the notion of dialectics, which refers to the idea that contradictory or opposing perspectives can both be true. In DBT, this is applied to the therapist-client relationship, where the therapist takes a non-judgemental stance and accepts the client as they are, while also encouraging change. The therapist and client work together to find a balance between acceptance and change in order to promote growth and healing.
DBT consists of several components that are typically delivered in weekly individual and group therapy sessions:
- Skills Training: Clients learn a set of practical skills to help them cope with distress and manage their emotions more effectively. These skills are divided into four modules: mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance.
- Therapy Sessions: Individual therapy sessions provide clients with a safe space to explore their thoughts, feelings, and behaviours. The therapist helps the client identify problematic patterns and develop strategies to address them.
- Phone Coaching: Clients have access to their therapist outside of scheduled sessions, allowing them to receive support and guidance during moments of crisis or distress.
- Consultation Team: DBT therapists meet regularly with a consultation team to ensure they are providing effective treatment. The team provides support and guidance to therapists to help them enhance their clinical skills.
By combining these different components, DBT aims to help individuals build a life worth living and improve their overall functioning. It emphasizes the importance of acceptance, validation, and self-compassion, while also promoting change and personal growth.
Research has shown that DBT can be highly effective in reducing self-harm behaviours, suicide attempts, and hospitalizations among individuals with BPD. It has also been shown to be helpful for other mental health conditions, particularly those characterized by emotional dysregulation.
Overall, DBT offers individuals a comprehensive approach to therapy that addresses both acceptance and change. It provides practical skills and strategies to help individuals cope with their emotions and improve their overall well-being. Whether you are struggling with BPD, depression, anxiety, or substance abuse, DBT may be a valuable tool in your journey towards recovery.
The History of Dialectical Behaviour Therapy
Dialectical Behaviour Therapy (DBT) was developed in the late 1980s by Dr. Marsha M. Linehan, a psychology researcher and therapist. Dr. Linehan initially developed DBT as a treatment for individuals with Borderline Personality Disorder (BPD) who were experiencing chronic suicidal ideation and self-harm behaviors.
Dr. Linehan recognized that traditional therapeutic approaches, such as cognitive-behavioral therapy (CBT), were not sufficient for individuals with BPD due to their high emotional intensity, difficulty regulating emotions, and interpersonal instability. As a result, she developed DBT, which combines elements of CBT with principles of acceptance and mindfulness.
DBT is heavily influenced by a philosophical framework known as dialectics. Dialectics refers to the idea that two seemingly contradictory concepts can coexist and be integrated to form a more complete understanding. In DBT, this concept is applied to help individuals find a balance between acceptance and change.
Over the years, DBT has expanded beyond its initial application for BPD and has been found to be effective in treating a range of mental health conditions, including substance use disorders, eating disorders, depression, and post-traumatic stress disorder (PTSD). The principles and techniques of DBT have also been adapted for use in both individual and group therapy settings.
Since its development, DBT has undergone several revisions and refinements. The original model, known as standard DBT, consisted of individual therapy, group skills training, telephone coaching, and therapist consultation teams. This comprehensive approach was found to be effective in reducing suicidal behaviors and improving emotion regulation skills.
Subsequent variations of DBT have been developed to meet the specific needs of different populations and settings. For example, DBT for adolescents (DBT-A) has been adapted to address the unique challenges faced by teenagers. DBT for couples (DBT-C) has also been developed to help couples improve their communication and relationship skills.
Overall, the history of DBT highlights the importance of individualizing treatment approaches to address the unique needs of individuals with complex and challenging mental health conditions. Through ongoing research and refinement, DBT continues to evolve and improve, offering hope and support to individuals seeking to improve their emotional well-being and quality of life.
Core Principles of Dialectical Behaviour Therapy
Dialectical Behaviour Therapy (DBT) is an evidence-based psychotherapy created by Dr. Marsha Linehan. It was originally developed to treat individuals with Borderline Personality Disorder (BPD), but has since been adapted to treat a range of mental health conditions. The therapy is based on several core principles that guide the treatment process and promote effective change.
1. Dialectics
DBT takes a dialectical approach, which means finding a balance between acceptance and change. The therapist and client work together to find a middle ground between accepting the client’s current reality and behavior, while also encouraging change and growth.
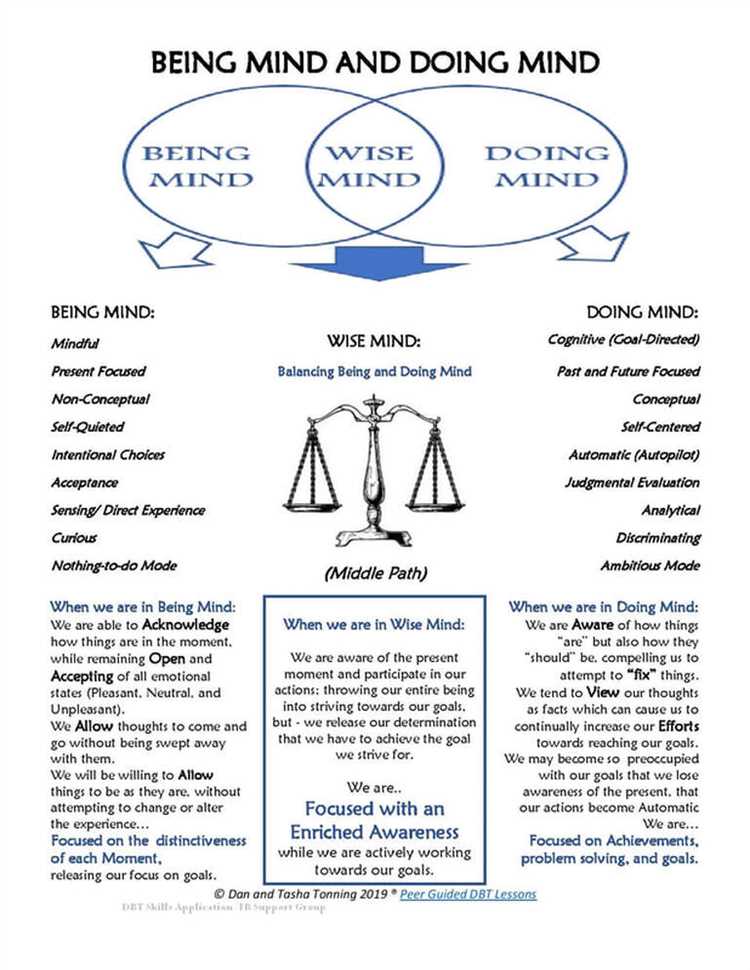
2. Mindfulness
Mindfulness is a key component of DBT. Clients are taught to become more aware of their thoughts, feelings, and bodily sensations in the present moment, without judgment. By practicing mindfulness, individuals can increase their ability to tolerate distress and make more intentional choices.
3. Distress Tolerance
DBT emphasizes the importance of learning and employing healthy coping skills to tolerate distressing situations. Clients are taught various techniques, such as self-soothing, relaxation exercises, and distraction strategies, to help them manage intense emotions and distress.
4. Emotional Regulation
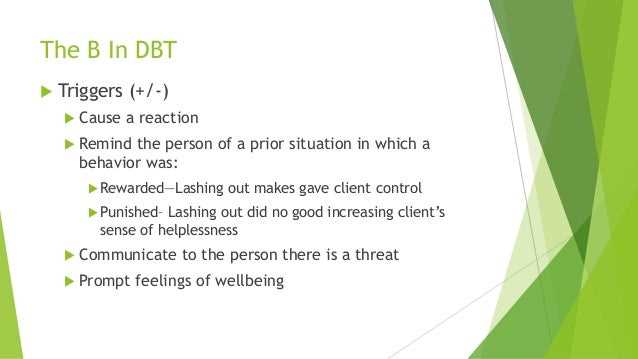
Emotional regulation skills are essential in DBT. Clients learn techniques to identify, understand, and manage their emotions in a healthy way. This involves increasing emotional awareness, identifying triggers, and developing strategies to effectively regulate intense emotions.
5. Interpersonal Effectiveness
Interpersonal effectiveness skills are taught in DBT to help clients improve their relationships and develop healthy communication skills. Clients learn how to set boundaries, assert their needs, and navigate conflicts effectively.
6. Validation
Validation is a core principle in DBT. Therapists aim to understand and acknowledge the client’s experience and emotions without judgment. Validation helps create a safe and supportive therapeutic environment and fosters a strong therapeutic alliance.
7. Consultation Team
DBT therapists often engage in regular consultation team meetings to ensure they are providing the best possible care to their clients. During these meetings, therapists discuss their caseloads and receive support and supervision from their colleagues.
8. Stage-Based Approach
DBT typically follows a stage-based approach, with each stage focusing on different therapeutic goals. The early stage focuses on achieving behavioral stability and reducing life-threatening behaviors, while the later stages target improving quality of life and increasing self-respect and self-esteem.
Conclusion
The core principles of Dialectical Behaviour Therapy provide a framework for therapists and clients to work together towards positive change. By incorporating dialectics, mindfulness, distress tolerance, emotional regulation, interpersonal effectiveness, validation, consultation team, and a stage-based approach, DBT offers a comprehensive and effective treatment approach for a range of mental health conditions.
Skills Taught in Dialectical Behaviour Therapy
Dialectical Behaviour Therapy (DBT) focuses on teaching individuals a set of skills that can help them manage their emotions, improve their relationships, and cope with stress and distress. These skills are divided into four main categories:
-
Mindfulness:
- Being present in the moment.
- Observing without judgment.
- Practicing acceptance of thoughts and feelings.
-
Distress Tolerance:
- Learning to tolerate distressing situations.
- Accepting reality as it is.
- Using crisis survival strategies.
-
Emotion Regulation:
- Understanding emotions and their functions.
- Identifying and labeling emotions.
- Increasing positive emotions and decreasing negative emotions.
- Changing emotions that are unwanted or unhelpful.
-
Interpersonal Effectiveness:
- Improving communication skills.
- Learning how to assert oneself.
- Setting boundaries.
- Building and maintaining healthy relationships.
These skills are taught through various techniques and exercises, such as individual therapy sessions, group skills training, phone coaching, and homework assignments. By learning and practicing these skills, individuals can develop more effective ways of handling difficult emotions, managing relationships, and navigating challenging situations.
Applying Dialectical Behaviour Therapy in Various Settings
Dialectical Behaviour Therapy (DBT) is a comprehensive and evidence-based therapeutic approach that was developed by Marsha M. Linehan. Originally designed for individuals with Borderline Personality Disorder (BPD), DBT has since been adapted and applied in various settings to address a wide range of mental health issues and behavioral patterns.
Here are some of the different settings in which DBT can be applied:
1. Outpatient Mental Health Clinics
DBT is commonly used in outpatient mental health clinics to treat individuals with a variety of mental health conditions, such as depression, anxiety disorders, eating disorders, substance use disorders, and self-harming behaviors. The skills taught in DBT, including mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness, can help individuals manage their symptoms and improve their overall well-being.
2. Inpatient Psychiatric Hospitals
DBT can also be implemented in inpatient psychiatric hospitals to provide intense and structured treatment for individuals with severe mental health conditions. This setting allows for a highly focused and supportive environment, where individuals can learn and practice the necessary skills to regulate their emotions, cope with distress, and enhance their relationships.
3. Schools and Educational Settings
DBT skills can be beneficial for students who struggle with emotional regulation, social skills, and academic performance. By incorporating DBT principles and strategies into the school curriculum, educators can help students develop effective coping mechanisms, improve their interpersonal communication, and enhance their overall emotional well-being.
4. Community Mental Health Programs
DBT can be implemented in community mental health programs to support individuals who may not have access to traditional outpatient therapy services. These programs can provide group therapy sessions and skill-building workshops, offering individuals a safe and supportive space to learn and practice the DBT skills necessary for managing their mental health.
5. Correctional Facilities
DBT has also been adapted for use in correctional facilities to help individuals involved in the criminal justice system manage their emotions, develop effective coping mechanisms, and reduce risk factors for recidivism. By teaching DBT skills to inmates, this approach aims to promote positive behavior change and support successful reintegration into society.
Overall, the versatility of DBT allows for its application in various settings, making it a valuable tool in addressing a wide range of mental health issues and behavioral patterns. Whether it’s in outpatient clinics, schools, or correctional facilities, DBT provides individuals with the skills they need to lead fulfilling and meaningful lives.
Effectiveness and Research of Dialectical Behaviour Therapy
Dialectical Behaviour Therapy (DBT) has been extensively studied and proven effective in treating a variety of mental health concerns. Research has shown that DBT is especially effective for individuals with borderline personality disorder (BPD), but it has also been shown to be beneficial for those with other conditions such as substance use disorders, eating disorders, post-traumatic stress disorder (PTSD), and depression.
Several randomized controlled trials have demonstrated the effectiveness of DBT in reducing suicidal and self-harming behaviors, improving emotion regulation, and enhancing overall quality of life. These studies have consistently shown that individuals who receive DBT experience greater reductions in self-destructive behaviors compared to those who receive other therapies or no treatment at all.
One of the key components of DBT is skills training, which helps individuals learn new coping strategies and improve their emotion regulation skills. Studies have found that this aspect of DBT is particularly helpful in reducing impulsive behaviors and promoting healthier emotional responses.
Furthermore, research has shown that the benefits of DBT are long-lasting, with individuals exhibiting continued improvement even after treatment has ended. This highlights the sustainability of the skills and strategies learned in therapy.
In addition to its effectiveness in clinical settings, DBT has also been adapted for use in various contexts, including schools, correctional facilities, and community-based programs. These adaptations have shown promising results in reducing aggressive behaviors, improving emotional well-being, and promoting prosocial behavior.
Overall, the body of research on DBT supports its effectiveness in treating a wide range of mental health conditions. The comprehensive and evidence-based approach of DBT, with its focus on enhancing skills and building a life worth living, makes it a valuable therapeutic tool for individuals seeking to improve their emotional well-being and overall functioning.
Common Challenges and Limitations in Dialectical Behaviour Therapy
Dialectical Behaviour Therapy (DBT) is a highly effective treatment for individuals with borderline personality disorder and other complex mental health conditions. However, like any therapy approach, it is not without its challenges and limitations. Being aware of these challenges can help therapists and clients anticipate and address them in the course of treatment.
1. Time and Resource Intensive
One of the main challenges of DBT is that it requires a significant commitment of time and resources. DBT typically involves individual therapy sessions, group skills training sessions, phone coaching between sessions, and weekly consultation team meetings among therapists. This level of intensity can be difficult for clients who have busy schedules or limited resources, making it challenging to fully participate in the therapy.
2. Resistance to Change
Another common challenge in DBT is client resistance to change. A core component of DBT is teaching clients new skills and strategies to cope with distressing emotions and problematic behaviors. However, some clients may be resistant to change due to fear, reluctance, or a lack of belief in their ability to change. Overcoming this resistance requires a strong therapeutic alliance and a supportive environment.
3. Emotional Dysregulation
DBT is particularly effective for individuals who struggle with emotional dysregulation, but this can also pose a challenge in the therapy process. Clients may become overwhelmed by their emotions during sessions, leading to difficulties in effectively engaging in therapy and practicing the skills they have learned. Therapists must be skilled in managing and navigating these intense emotional moments to ensure progress in therapy.
4. Limited Generalizability
While DBT has been shown to be effective in treating borderline personality disorder, it may be less effective for individuals with different diagnoses or less severe symptoms. The skills and strategies taught in DBT may not always generalize to other settings or situations, which can limit the overall effectiveness of the therapy for some clients. Supplementing DBT with other treatment approaches may be necessary in these cases.
5. Therapist Competence
DBT is a complex and specialized therapy approach that requires therapists to undergo extensive training and supervision. However, there may be a shortage of trained and competent DBT therapists, particularly in some areas or healthcare systems. A lack of therapist competence or adherence to the principles of DBT can limit the effectiveness of the therapy for clients.
6. Stigma and Accessibility
Lastly, stigma and accessibility can also be barriers to receiving DBT treatment. Some individuals may be hesitant to seek DBT due to the stigma associated with mental health treatment, particularly for conditions like borderline personality disorder. Additionally, limited access to DBT services, either due to geographical location or financial barriers, can prevent individuals from receiving the therapy they may need.
Despite these challenges and limitations, DBT remains a highly effective and evidence-based therapy for individuals with borderline personality disorder and other complex mental health conditions. With proper support and adaptations, many of these challenges can be overcome to ensure successful treatment outcomes.
Questions and answers
What is Dialectical Behaviour Therapy (DBT)?
Dialectical Behaviour Therapy (DBT) is a type of therapy that combines cognitive-behavioral techniques with strategies from Eastern mindfulness practices. It was originally developed to help individuals who struggled with self-destructive behaviors and borderline personality disorder.
Who can benefit from Dialectical Behaviour Therapy?
Dialectical Behaviour Therapy can benefit individuals who struggle with self-destructive behaviors, such as self-harm, suicidal thoughts, substance abuse, or eating disorders. It can also be helpful for those with borderline personality disorder, depression, anxiety, or other mental health conditions.
What are some of the key components of Dialectical Behaviour Therapy?
Some key components of Dialectical Behaviour Therapy include individual therapy sessions, group skills training, phone coaching, and therapist consultation teams. The therapy focuses on four main skills: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
How does Dialectical Behaviour Therapy differ from other types of therapy?
Dialectical Behaviour Therapy differs from other types of therapy in its emphasis on acceptance and change. It combines acceptance-based strategies with concrete skills training to help individuals create a life worth living. It also incorporates mindfulness practices, which can help individuals become more aware of their thoughts, emotions, and behaviors.
Is Dialectical Behaviour Therapy effective?
Yes, research has shown that Dialectical Behaviour Therapy can be highly effective in reducing self-destructive behaviors, improving emotion regulation, and enhancing overall functioning. It has been found to be particularly helpful for individuals with borderline personality disorder, but it can also benefit those with other mental health conditions.