Bipolar disorder and borderline personality disorder are two mental health conditions that can significantly impact a person’s life. While there may be some similarities between the two disorders, it is vital to understand the differences and the various treatment options available for each.
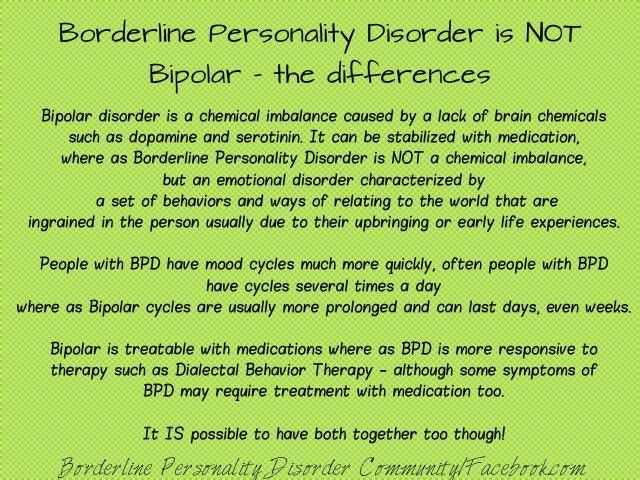
Bipolar disorder, also known as manic depressive disorder, is characterized by extreme mood swings, ranging from manic episodes of heightened energy and euphoria to depressive episodes of sadness and hopelessness. These mood swings can occur over a period of days, weeks, or even months, and can greatly disrupt a person’s daily functioning and relationships.
On the other hand, borderline personality disorder is characterized by unstable moods, self-image, and relationships. Individuals with borderline personality disorder often experience intense episodes of anger, anxiety, and depression that can last for hours or days. They may also engage in impulsive and risky behaviors and have an intense fear of abandonment.
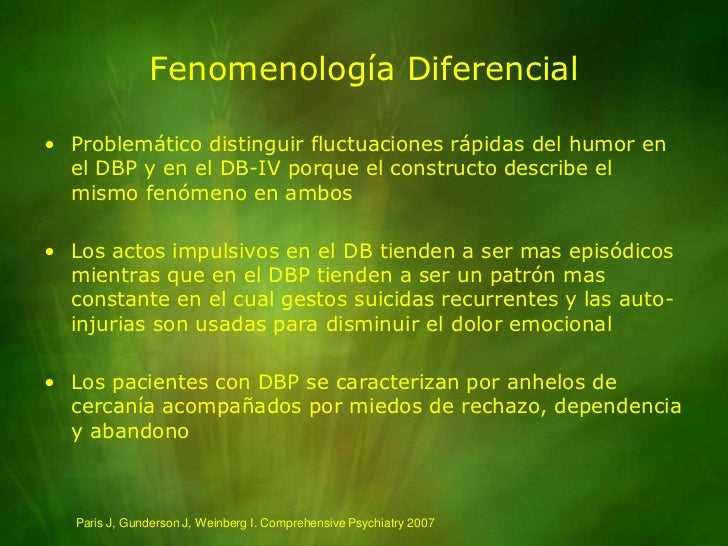
While both disorders involve mood instability, the main difference lies in the duration and intensity of the symptoms. Bipolar disorder is typically characterized by longer-lasting and more extreme mood swings, while borderline personality disorder is characterized by rapid, intense shifts in mood and self-perception.
Treatment options for bipolar disorder often involve a combination of medication, therapy, and lifestyle changes. Mood stabilizers, antidepressants, and antipsychotic medications may be prescribed to help manage symptoms. Additionally, therapy can help individuals with bipolar disorder develop coping mechanisms and improve their overall quality of life.
Treatment for borderline personality disorder may include a combination of medication and therapy as well. Antidepressant or antianxiety medications may be prescribed to help manage symptoms, and dialectical behavior therapy (DBT) or cognitive-behavioral therapy (CBT) may be implemented to help individuals develop healthier coping mechanisms and improve interpersonal skills.
Overall, understanding the differences between bipolar disorder and borderline personality disorder is essential for accurate diagnosis and effective treatment. While both conditions can be challenging to manage, proper treatment can significantly improve a person’s quality of life and help them lead a more fulfilling and stable existence.
Bipolar Disorder vs Borderline Personality Disorder
Bipolar disorder and borderline personality disorder (BPD) are two mental health conditions that can significantly impact an individual’s thoughts, emotions, and behavior. While they can share similar symptoms, they are distinct disorders with different underlying causes and treatment approaches.
Symptoms and Characteristics
- Bipolar Disorder: Bipolar disorder is characterized by episodes of extreme mood swings, including manic episodes and depressive episodes. During manic episodes, individuals may experience elevated mood, increased energy, racing thoughts, and impulsive behavior. Depressive episodes are characterized by sadness, lack of energy, loss of interest in activities, and difficulty concentrating.
- Borderline Personality Disorder: BPD is characterized by difficulties with emotions, self-image, and interpersonal relationships. Individuals with BPD may have unstable relationships, intense fear of abandonment, impulsive behavior, chronic feelings of emptiness, and recurrent suicidal thoughts or self-harming behaviors.
Underlying Causes
- Bipolar Disorder: The exact cause of bipolar disorder is unclear, but it is believed to be a combination of genetic, environmental, and neurological factors. There may be a genetic predisposition, as individuals with a family history of bipolar disorder are more likely to develop the condition.
- Borderline Personality Disorder: BPD is thought to develop from a combination of genetic, environmental, and interpersonal factors. Traumatic experiences or a history of childhood abuse or neglect can also contribute to the development of BPD.
Treatment Options
Bipolar Disorder: Treatment for bipolar disorder typically involves a combination of medication, such as mood stabilizers and antidepressants, and therapy, such as cognitive-behavioral therapy (CBT) or dialectical behavior therapy (DBT). Psychoeducation about the condition and lifestyle adjustments, such as maintaining a regular sleep schedule and reducing stress, are also important components of bipolar disorder management.
Borderline Personality Disorder: Treatment for BPD often includes a combination of psychotherapy, such as dialectical behavior therapy (DBT), cognitive-behavioral therapy (CBT), and psychodynamic therapy. Medication may also be prescribed to manage specific symptoms or co-occurring disorders, such as depression or anxiety. Building healthy coping skills, stress management techniques, and establishing stable relationships are essential for individuals with BPD.
Conclusion
While both bipolar disorder and borderline personality disorder can cause significant disturbances in an individual’s life, understanding the differences in symptoms, underlying causes, and treatment options is crucial. Proper diagnosis and appropriate treatment can help individuals with these conditions lead fulfilling and productive lives.
Understanding Bipolar Disorder
Bipolar disorder, also known as manic-depressive illness, is a mental disorder characterized by extreme shifts in mood, energy, and activity levels. People with bipolar disorder experience episodes of mania, which is characterized by elevated mood, increased energy, and impulsive behavior, as well as episodes of depression, characterized by feelings of sadness, low energy, and loss of interest in activities.
Some common symptoms of bipolar disorder include:
- Mood swings from extreme highs (mania) to extreme lows (depression)
- Increased energy levels during manic episodes
- Feelings of restlessness or being on edge
- Irritability and agitation
- Decreased need for sleep
- Racing thoughts and rapid speech
- Engaging in risky behaviors
- Loss of interest in activities during depressive episodes
- Feelings of hopelessness and worthlessness
- Changes in appetite and weight
Bipolar disorder can affect anyone, regardless of age, gender, or background. It often begins in adolescence or early adulthood, although some people may experience symptoms in childhood or later in life.
The exact cause of bipolar disorder is unknown, but it is believed to be a combination of genetic and environmental factors. Research suggests that imbalances in certain brain chemicals, such as neurotransmitters like serotonin and dopamine, may play a role in the development of the disorder.
Treatment for bipolar disorder typically involves a combination of medication and therapy. Mood stabilizers, such as lithium or anticonvulsant drugs, are often prescribed to help manage manic and depressive symptoms. Therapy, such as cognitive-behavioral therapy (CBT) or psychoeducation, can help individuals learn coping skills and manage their symptoms.
It is important for individuals with bipolar disorder to work closely with a healthcare provider to develop an appropriate treatment plan and to monitor their symptoms. With proper treatment and support, most people with bipolar disorder can lead healthy and productive lives.
Understanding Borderline Personality Disorder
Borderline Personality Disorder (BPD) is a mental health condition characterized by intense emotional instability, difficulty in maintaining healthy relationships, and a distorted self-image. It is a long-term condition that can cause significant distress and impairment in daily functioning.
Some key characteristics of individuals with BPD include:
- Unstable and intense relationships, often marked by idealization and devaluation
- Impulsive and reckless behavior, such as substance abuse and self-harm
- Emotional instability, including frequent mood swings and intense anger
- Chronic feelings of emptiness and loneliness
- Distorted self-image and unstable sense of identity
- Fear of abandonment and efforts to avoid real or imagined abandonment
Diagnosing BPD can be challenging, as its symptoms can overlap with other mental health conditions. However, mental health professionals typically rely on a detailed assessment and evaluation of the individual’s symptoms and history to make an accurate diagnosis.
While the exact cause of BPD is unknown, researchers believe that a combination of genetic, environmental, and neurobiological factors contribute to its development. Childhood trauma, such as physical or sexual abuse, neglect, or unstable family environments, is often associated with the development of BPD.
Treatment for BPD often involves a combination of therapy and medication. Psychotherapy, specifically dialectical behavior therapy (DBT), is considered the most effective treatment for BPD. DBT focuses on teaching individuals coping skills to manage intense emotions, improve interpersonal relationships, and regulate impulsive behaviors.
In addition to therapy, medications such as antidepressants, mood stabilizers, or antipsychotics may be prescribed to help manage specific symptoms of BPD, such as depression, anxiety, or impulsivity.
Living with BPD can be challenging, but with proper diagnosis, treatment, and support, individuals with the disorder can learn to manage their symptoms, have healthier relationships, and lead fulfilling lives.
Differences between Bipolar Disorder and Borderline Personality Disorder
Bipolar Disorder
- Bipolar disorder is a mood disorder characterized by extreme shifts in mood, energy, and activity levels.
- These shifts are usually separated into manic episodes and depressive episodes.
- Manic episodes are characterized by elevated mood, increased energy and activity, racing thoughts, impulsivity, and reduced need for sleep.
- Depressive episodes are characterized by feelings of sadness, low energy, decreased interest in activities, changes in appetite and sleep patterns, and thoughts of death or suicide.
- Bipolar disorder is typically a chronic condition that requires ongoing treatment and management.
- Treatment options for bipolar disorder often include a combination of medication, therapy, and lifestyle changes.
Borderline Personality Disorder
- Borderline personality disorder is a personality disorder characterized by instability in mood, self-image, and relationships.
- Individuals with borderline personality disorder often experience intense and unstable emotions, impulsivity, fear of abandonment, and difficulty controlling anger.
- They may also engage in self-destructive behaviors, have distorted self-image, and experience chronic feelings of emptiness.
- Borderline personality disorder is also often associated with a history of trauma or abuse.
- Treatment options for borderline personality disorder typically involve therapy, such as dialectical behavior therapy (DBT), which focuses on developing coping skills and emotional regulation.
| Characteristic | Bipolar Disorder | Borderline Personality Disorder |
|---|---|---|
| Key Features | Extreme mood swings, manic and depressive episodes | Intense emotional instability, fear of abandonment, self-destructive behavior |
| Duration | Chronic condition, requiring ongoing treatment | Chronic condition, often improves with age |
| Treatment Options | Medication, therapy, lifestyle changes | Therapy, particularly DBT |
| Associated Factors | N/A | History of trauma or abuse |
Similarities between Bipolar Disorder and Borderline Personality Disorder
Bipolar disorder and borderline personality disorder (BPD) share some similarities in terms of symptoms and characteristics. Understanding these similarities can help in differentiating between the two disorders and providing appropriate treatment.
| Bipolar Disorder | Borderline Personality Disorder |
|---|---|
|
|
Both disorders also have an onset in late adolescence or early adulthood and can significantly interfere with daily functioning and relationships. It is important to note that while there are similarities, there are also important differences in terms of treatment approaches and underlying causes. Bipolar disorder is primarily treated with mood stabilizers, whereas BPD typically requires a combination of therapies, such as dialectical behavior therapy (DBT), medication, and psychotherapy.
Treatment Options for Bipolar Disorder
Treatment for bipolar disorder often involves a combination of medication, therapy, and lifestyle changes. The specific approach will vary depending on the individual’s symptoms and needs.
Medication: Mood stabilizers, such as lithium or valproate, are commonly prescribed to help manage the extreme mood swings associated with bipolar disorder. Antipsychotic medications may also be used to regulate mood and manage psychotic symptoms. Antidepressants may be prescribed cautiously in certain cases, as they can potentially trigger manic episodes.
Therapy: Psychotherapy, also known as talk therapy, can be instrumental in helping individuals with bipolar disorder manage their symptoms and build coping skills. Cognitive-behavioral therapy (CBT) is often used to identify and change negative thought patterns and behaviors. Interpersonal and social rhythm therapy (IPSRT) can help individuals develop regular routines and maintain stability in their daily lives.
Lifestyle Changes: Adopting a healthy lifestyle can have a positive impact on managing bipolar disorder. Regular sleep patterns, a balanced diet, and regular exercise can help stabilize mood and overall well-being. Avoiding drugs and alcohol is also crucial, as substance abuse can worsen symptoms.
Support Network: Building a strong support network can be beneficial for individuals with bipolar disorder. This may include friends, family members, support groups, and healthcare professionals who can offer guidance, understanding, and support throughout the treatment process.
Monitoring and Adjusting Treatment: Regular monitoring of symptoms and medication effectiveness is crucial in managing bipolar disorder. It may be necessary to adjust medication dosages or try different medications to find the most effective treatment plan for an individual.
Continued Treatment: Bipolar disorder is a chronic condition that typically requires long-term treatment. It is important for individuals to continue their treatment plan even during periods of stability to prevent relapse and maintain overall well-being.
Collaborative Approach: Treatment for bipolar disorder often involves a collaborative approach between the individual, their healthcare provider, and any other professionals involved in their care. Regular communication and open dialogue can help ensure that treatment goals are being met and any concerns or changes in symptoms are addressed promptly.
Treatment Options for Borderline Personality Disorder
Borderline Personality Disorder (BPD) is a complex mental health condition that requires comprehensive treatment. While there is no cure for BPD, there are several treatment options available to help individuals manage their symptoms, improve their overall well-being, and enhance their ability to live fulfilling lives.
- Psychotherapy: Psychotherapy, specifically Dialectical Behavior Therapy (DBT), is considered the gold standard treatment for BPD. DBT focuses on teaching individuals skills to manage intense emotions, improve relationships, and regulate impulsive behaviors. Individual therapy sessions and group therapy are usually components of this therapy.
- Medication: Although medication is not a primary treatment for BPD, it can be helpful in managing specific symptoms that coexist with the disorder. Antidepressants, mood stabilizers, and antipsychotic medications may be prescribed to target symptoms such as depression, anxiety, and mood swings.
- Self-Care: Engaging in self-care activities is essential for individuals with BPD. This can include practicing mindfulness and relaxation techniques, engaging in regular exercise, maintaining a balanced diet, and getting enough sleep. Self-care activities can help individuals manage stress, reduce emotional dysregulation, and improve overall well-being.
- Social Support: Building and maintaining a strong support system is crucial for individuals with BPD. Having trusted friends, family members, or support groups can provide emotional support, understanding, and validation. Social support systems can help reduce feelings of isolation and provide a sense of belonging.
- Education: Increasing knowledge and understanding about BPD can help individuals and their loved ones navigate the challenges associated with the disorder. Learning about the symptoms, causes, and treatment options can provide individuals with a sense of empowerment and help them make informed decisions about their care.
- Complementary Therapies: Some individuals with BPD find complementary therapies helpful in managing their symptoms. These may include practices such as yoga, meditation, art therapy, and acupuncture. While not a substitute for evidence-based treatments, complementary therapies can be used as additional tools for coping and self-expression.
It’s important for individuals with BPD to work closely with mental health professionals to create a personalized treatment plan that addresses their specific needs and goals. With the right combination of treatments and support, individuals with BPD can experience significant improvements in their quality of life.
Questions and answers
What is bipolar disorder?
Bipolar disorder is a mental illness characterized by extreme mood swings, ranging from periods of mania to periods of depression.
How does borderline personality disorder differ from bipolar disorder?
Borderline personality disorder is a mental illness characterized by unstable moods, intense and unstable relationships, and a strong fear of abandonment, whereas bipolar disorder is characterized by extreme mood swings.
What are the treatment options for bipolar disorder?
Treatment options for bipolar disorder may include medication, therapy, and lifestyle changes. Medications such as mood stabilizers and antipsychotics can help manage symptoms, and therapy can help individuals develop coping strategies and improve their overall well-being.
Can borderline personality disorder and bipolar disorder coexist?
Yes, it is possible for someone to have both borderline personality disorder and bipolar disorder. This is known as a dual diagnosis and may require a specialized treatment approach.
How is bipolar disorder diagnosed?
Bipolar disorder is diagnosed through a comprehensive evaluation, which may include a physical exam, psychiatric assessment, and a review of the individual’s medical and family history. A mental health professional will assess the presence and severity of symptoms to make an accurate diagnosis.
Are there any specific triggers for bipolar disorder?
While the exact cause of bipolar disorder is unknown, certain factors may contribute to the development or worsening of symptoms. These can include stressful life events, changes in sleep patterns, substance abuse, and certain medications. It’s important for individuals with bipolar disorder to be aware of these triggers and take steps to manage them.
What are some common symptoms of borderline personality disorder?
Common symptoms of borderline personality disorder include intense fear of abandonment, unstable relationships, impulsive behavior, emotional instability, and a distorted sense of self. Individuals with this disorder may also experience chronic feelings of emptiness and engage in self-destructive behaviors.