Borderline Personality Disorder (BPD) is a mental health condition characterized by intense emotional instability, impulsivity, and difficulty maintaining stable relationships. It affects approximately 1.4% of the adult population in the United States, making it a relatively common condition.
If you or a loved one has been diagnosed with BPD, it’s important to remember that help is available. There are many resources and support groups that can provide you with the guidance and assistance you need to navigate the challenges of living with BPD.
One of the most effective forms of treatment for BPD is therapy. There are several types of therapy that have been shown to be beneficial for individuals with BPD, including dialectical behavior therapy (DBT), cognitive-behavioral therapy (CBT), and psychodynamic therapy. These therapies can help individuals with BPD gain a better understanding of their emotions, develop coping mechanisms, and improve their interpersonal skills.
Understanding Borderline Personality Disorder
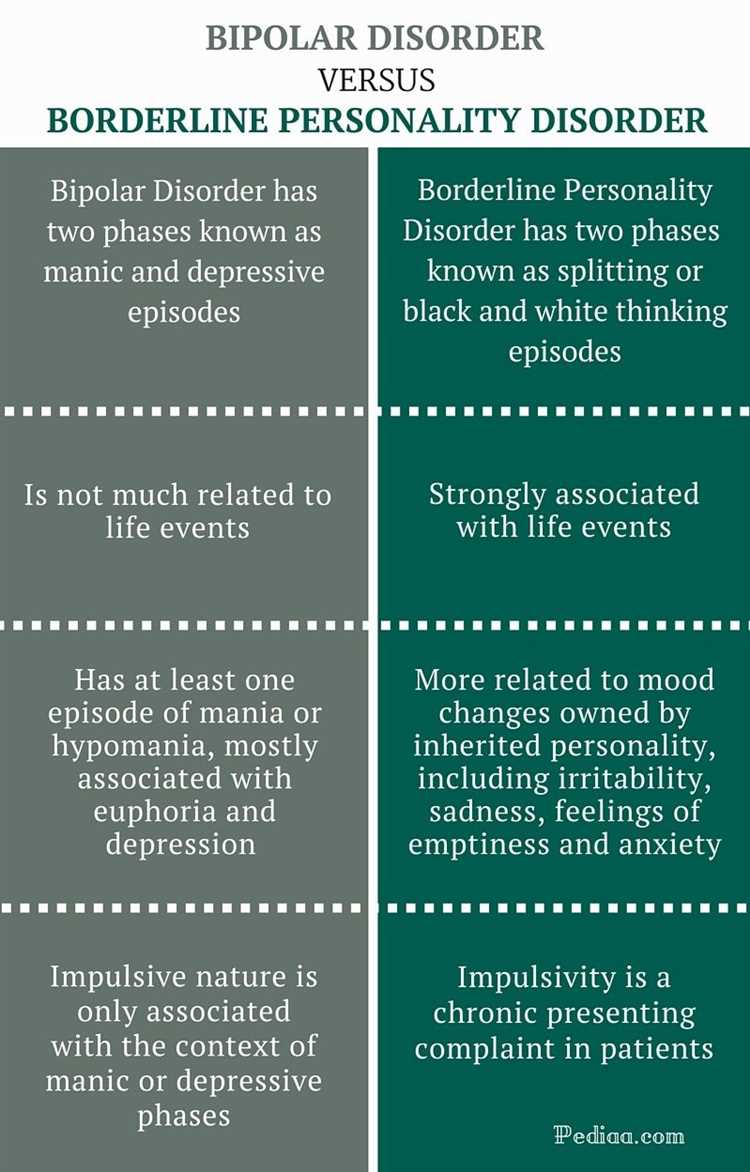
Borderline Personality Disorder (BPD) is a mental health condition that affects the way a person thinks, feels, and behaves. It is characterized by intense, unstable emotions, problematic relationships, and a distorted sense of self. People with BPD often struggle with controlling their emotions and may engage in impulsive and self-destructive behaviors. It is important to understand that BPD is a complex disorder and can vary in severity from person to person.
Here are some key points to help you better understand Borderline Personality Disorder:
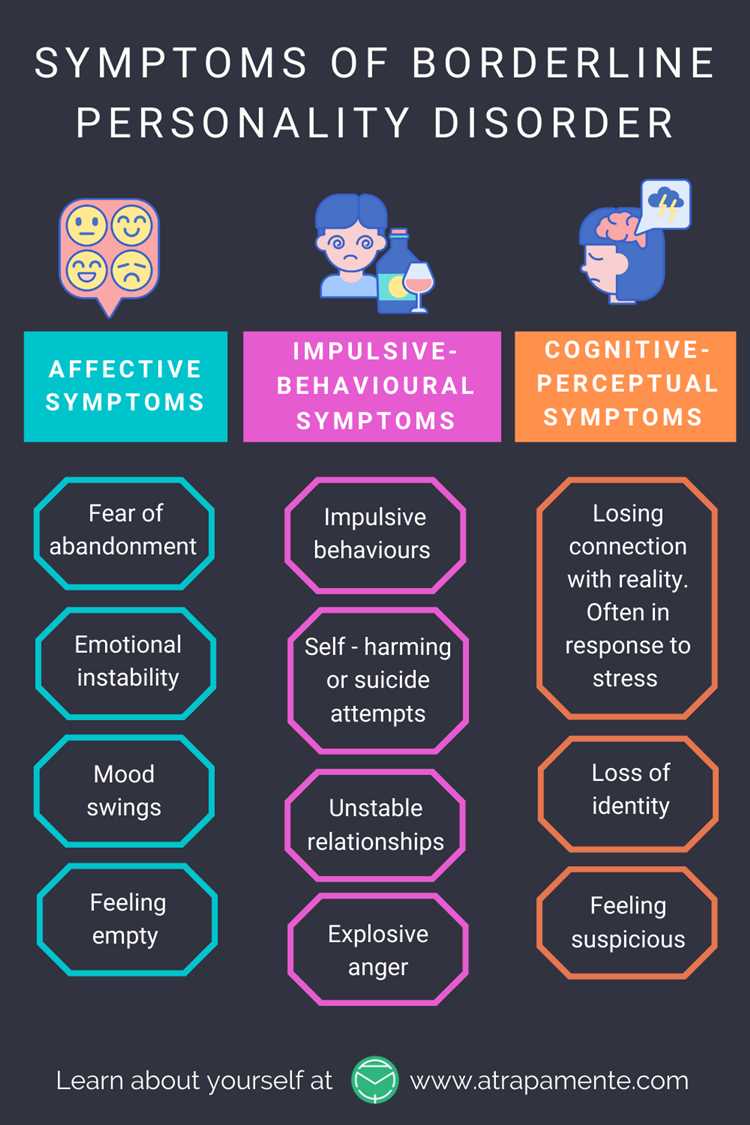
- Symptoms: The symptoms of BPD can manifest in various ways, but some common ones include: intense fear of abandonment, unstable relationships, identity disturbance, chronic feelings of emptiness, impulsivity, self-harm, and emotional instability.
- Causes: The exact cause of BPD is not known, but research suggests that a combination of genetic, environmental, and neurological factors may contribute to its development. Trauma and invalidating environments during childhood are also thought to play a role.
- Diagnosis: BPD is diagnosed by a mental health professional based on a thorough assessment of symptoms and personal history. It is important to consult with a qualified healthcare provider for an accurate diagnosis.
- Treatment: While there is no cure for BPD, several treatment options can help manage symptoms and improve quality of life. These may include psychotherapy (such as dialectical behavior therapy), medication, support groups, and self-help strategies.
- Self-Help Strategies: There are several self-help strategies that can be effective in managing BPD symptoms. These may include practicing mindfulness and relaxation techniques, maintaining a balanced lifestyle, developing healthy coping mechanisms, and fostering supportive relationships.
- Support: Building a strong support network is crucial for individuals with BPD. This may involve reaching out to family, friends, and support groups for understanding, empathy, and practical assistance.
It is essential to seek professional help if you suspect you or someone you know may have Borderline Personality Disorder. Early intervention and appropriate treatment can make a significant difference in managing the condition and improving overall well-being.
Remember, BPD is a complex disorder, and each person’s experience with it is unique. It is important to approach the topic with empathy, understanding, and the goal of reducing stigma surrounding mental health.
Symptoms and Diagnosis
Borderline personality disorder (BPD) is a mental health condition that is characterized by a pattern of intense and unstable interpersonal relationships, self-image, and emotions. People with BPD often have difficulty regulating their emotions, which can lead to impulsive behavior and unstable moods.
Some of the common symptoms of BPD include:
- Extreme fear of abandonment
- Unstable relationships, which can involve alternating between idealizing and devaluing others
- Impulsive and self-destructive behaviors, such as self-harm, substance abuse, or reckless spending
- Intense and rapidly changing emotions, including anger, sadness, and anxiety
- Chronic feelings of emptiness
- Identity disturbance, or a persistent sense of self that is unstable or fluctuating
- Difficulty trusting others
- Paranoia or dissociation
Diagnosing BPD can be challenging because many of its symptoms can overlap with other mental health conditions. A mental health professional, such as a psychiatrist or psychologist, can evaluate a person’s symptoms and medical history to make an accurate diagnosis. They may use various diagnostic criteria, such as the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), to determine if someone meets the criteria for BPD.
It is important to note that a proper diagnosis should be made by a qualified professional. Self-diagnosis or relying solely on internet resources is not recommended.
Once a diagnosis is made, a treatment plan can be developed. Treatment for BPD often involves a combination of psychotherapy, medication, and support. Psychotherapy, such as dialectical behavior therapy (DBT), can help individuals learn skills to manage their emotions, improve relationships, and reduce impulsive behaviors. Medication may be prescribed to help manage specific symptoms, such as depression or anxiety. Additionally, having a strong support system can be crucial in managing BPD, whether it’s through family, friends, or support groups.
If you suspect that you or someone you know may have BPD, it is important to seek professional help. A mental health professional can provide an accurate diagnosis and help develop a treatment plan that best suits the individual’s needs.
Causes and Risk Factors
Borderline Personality Disorder (BPD) is a complex mental health condition that arises from a combination of genetic, environmental, and psychological factors. While the exact cause of BPD is still unknown, researchers have identified several potential risk factors that may increase the likelihood of developing the disorder.
1. Genetics: People with a family history of BPD are more likely to develop the disorder themselves. This suggests a genetic component to the condition, although specific genes that contribute to BPD have not yet been identified.
2. Childhood Trauma: Individuals who have experienced traumatic events during childhood, such as physical or sexual abuse, neglect, or unstable family environments, may be at a higher risk of developing BPD. These traumatic experiences can disrupt the development of emotional regulation and interpersonal skills, contributing to the development of BPD later in life.
3. Environmental Factors: Certain environmental factors, such as growing up in an invalidating or chaotic family environment, may increase the likelihood of developing BPD. Invalidating environments are characterized by a lack of emotional support, inconsistent or unpredictable responses, and a dismissal or denial of a person’s feelings or experiences.
4. Neurobiological Factors: Some studies suggest that individuals with BPD may have abnormalities in brain structure and function, particularly in areas related to emotional regulation and impulse control. These neurobiological factors may contribute to the symptoms and behaviors associated with BPD.
5. Co-occurring Mental Health Disorders: BPD often co-occurs with other mental health disorders, such as depression, anxiety disorders, substance abuse, and eating disorders. The presence of these co-occurring disorders may increase the risk of developing BPD or exacerbate existing symptoms.
6. Personality Traits: Certain personality traits, such as impulsivity, emotional lability, and difficulties in regulating emotions, may be predisposing factors for BPD. These traits can contribute to the development of BPD when combined with other risk factors.
It’s important to note that having one or more of these risk factors does not guarantee the development of BPD. Many individuals with these risk factors do not develop BPD, while others without these risk factors may still develop the disorder. BPD is a complex condition that arises from a combination of factors, and further research is needed to fully understand its causes.
Treatment Options
There are several treatment options available for individuals with Borderline Personality Disorder (BPD). The most common forms of treatment include:
- Psychotherapy: Psychotherapy is a type of talk therapy that involves working with a mental health professional to identify and address the underlying issues and behavioral patterns associated with BPD. Different types of psychotherapy approaches, such as dialectical behavior therapy (DBT), cognitive-behavioral therapy (CBT), and psychodynamic therapy, may be used to help individuals with BPD.
- Medication: Medications can be helpful in managing specific symptoms associated with BPD, such as depression, anxiety, and impulsivity. Antidepressant, mood stabilizer, and antipsychotic medications may be prescribed by a psychiatrist to help alleviate these symptoms.
- Supportive services: Supportive services, such as support groups or peer support programs, can provide individuals with BPD with a safe space to share their experiences, gain emotional support, and learn coping strategies from others who have similar experiences.
It is important to note that treatment for BPD is typically individualized based on the specific needs and circumstances of each person. A combination of treatments may be recommended, and the effectiveness of treatment can vary from person to person.
If you or someone you know is struggling with Borderline Personality Disorder, it is important to reach out to a mental health professional for an accurate diagnosis and appropriate treatment plan. With the right support and treatment, individuals with BPD can develop healthier coping skills and improve their overall well-being.
Therapy Approaches
When it comes to treating Borderline Personality Disorder (BPD), therapy plays a crucial role in helping individuals manage their symptoms and improve their overall well-being. Various therapy approaches have been developed to address the specific needs and challenges of individuals with BPD. Some of the most commonly used therapy approaches for BPD include:
- Dialectical Behavior Therapy (DBT): Developed specifically for individuals with BPD, DBT combines elements of cognitive-behavioral therapy (CBT) with mindfulness techniques. It focuses on teaching individuals skills to regulate emotions, tolerate distress, improve interpersonal relationships, and develop a sense of self-identity.
- Cognitive-Behavioral Therapy (CBT): CBT helps individuals with BPD identify and change negative thought patterns and behaviors. It aims to address distorted beliefs and develop healthier coping mechanisms. CBT can be effective in reducing impulsive behaviors, self-harm, and suicidal tendencies.
- Schema-Focused Therapy: This therapy approach targets maladaptive schemas or deeply ingrained patterns of thoughts and behaviors. It helps individuals with BPD understand and challenge these negative schemas and develop healthier alternatives.
- Psychodynamic Therapy: Psychodynamic therapy explores the underlying causes of BPD by focusing on unconscious thoughts and early life experiences. It aims to build self-awareness, improve emotional regulation, and enhance interpersonal skills.
- Transference-Focused Psychotherapy (TFP): TFP is a specialized form of psychodynamic therapy that emphasizes exploring and analyzing the relationship between the therapist and the individual with BPD. It aims to increase self-awareness, promote emotional regulation, and develop healthier interpersonal relationships.
In addition to these therapy approaches, group therapy and family therapy can also be beneficial for individuals with BPD. Group therapy provides a supportive environment where individuals can learn from others with similar experiences and gain additional insight into their own thoughts and behaviors. Family therapy helps improve communication and understanding among family members, reducing conflict and providing a more supportive environment for the individual with BPD.
It’s important to note that therapy approaches may be combined or tailored to meet the individual needs of each person with BPD. A qualified mental health professional can determine the most appropriate therapy approach and develop a personalized treatment plan.
Medications for Borderline Personality Disorder
Medications are often used as part of a comprehensive treatment plan for individuals with borderline personality disorder (BPD). While medications cannot treat BPD directly, they can help in managing certain symptoms and co-occurring conditions that often accompany BPD.
1. Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to individuals with BPD to help regulate mood and reduce symptoms of depression and anxiety. Some examples of SSRIs include fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro).
2. Mood stabilizers: Mood stabilizers, such as lithium or lamotrigine, are sometimes used to help stabilize mood swings and impulsive behaviors that are characteristic of BPD. These medications can help reduce the frequency and intensity of mood episodes.
3. Antipsychotics: Antipsychotic medications may be prescribed to individuals with BPD who experience symptoms such as psychosis, severe mood swings, or intense anger. These medications can help manage these symptoms and improve overall functioning.
4. Anti-anxiety medications: Anti-anxiety medications, such as benzodiazepines, may be prescribed on a short-term basis to help manage acute symptoms of anxiety or panic attacks. However, long-term use of benzodiazepines can be problematic and should be monitored closely.
5. Sleep aids: Sleep disturbances are common in individuals with BPD. Prescription sleep aids, such as zolpidem (Ambien), may be used to help improve sleep quality and reduce insomnia.
It’s important to note that medication should always be used in conjunction with therapy and other forms of support. Medications alone are unlikely to provide a complete solution for BPD, but they can be a helpful tool in managing specific symptoms and improving overall well-being.
Disclaimer: This article is for informational purposes only and should not be considered as medical advice. Consult with a healthcare professional for personalized recommendations.
Coping Strategies and Support
Living with borderline personality disorder (BPD) can be challenging, but there are coping strategies and support available to help you manage the symptoms and improve your well-being. Here are some strategies and resources to consider:
1. Psychotherapy
Psychotherapy, such as dialectical behavior therapy (DBT), is the most effective treatment for BPD. It focuses on teaching you skills to manage intense emotions, improve relationships, and build a more stable sense of self. Seeking out a qualified therapist who specializes in BPD can greatly benefit your recovery journey.
2. Self-care
Engaging in self-care activities can help provide a sense of calm and stability. Taking care of your physical health by eating a balanced diet, getting regular exercise, and getting enough sleep can positively impact your mental well-being. Additionally, incorporating relaxation techniques, such as deep breathing exercises or meditation, into your daily routine can help you manage stress and reduce anxiety.
3. Supportive relationships
Building and maintaining a support network of understanding family members, friends, or support groups can provide a sense of validation and understanding. Discussing your feelings and experiences with trusted individuals who can listen without judgment can offer emotional support and help you feel less alone in your struggles.
4. Education and self-help resources
Learning more about BPD can empower you to better understand your condition and develop effective coping strategies. There are many books, websites, and online forums dedicated to BPD that can provide you with valuable insights and tips for managing the symptoms. However, it is important to ensure that the information comes from reputable sources.
5. Crisis hotline
If you are experiencing a crisis or feeling overwhelmed, consider reaching out to a crisis hotline or helpline. These services provide immediate support and can help you navigate through difficult emotions. Save the hotline numbers in your phone or keep them accessible for quick access when needed.
6. Medication
In some cases, medication may be prescribed to help manage specific symptoms of BPD, such as anxiety or depression. It is important to discuss with a psychiatrist or mental health professional to determine if medication is a suitable option for you.
Remember, finding the right coping strategies and support may take time and experimentation. It is important to be patient and persistent in seeking out resources and strategies that work best for you.
Supporting Loved Ones with Borderline Personality Disorder
Borderline Personality Disorder (BPD) can have a significant impact on not only the individual diagnosed with it but also their loved ones. If someone you care about has BPD, it is important to provide them with understanding, empathy, and support. Here are some ways you can support your loved one with BPD:
- Educate yourself: Learn about BPD, its symptoms, and treatment options. This will help you understand what your loved one is going through and how to effectively support them.
- Practice active listening: Be present and actively listen when your loved one is sharing their thoughts and feelings with you. Avoid judgment and refrain from providing unsolicited advice.
- Validate their emotions: BPD often involves intense emotions that can be overwhelming for the individual. Validate their feelings, even if you may not fully understand or agree with them. Let them know that their emotions are valid and that you are there to support them.
- Encourage professional help: Encourage your loved one to seek professional help from a therapist or psychiatrist who specializes in BPD. Offer to help them find a suitable healthcare professional and accompany them to appointments if needed.
- Support self-care: Encourage your loved one to engage in self-care activities that promote their well-being, such as exercising, practicing mindfulness, or pursuing hobbies. Offer to participate in these activities together.
- Establish boundaries: It is essential to set boundaries to protect your own mental health while supporting your loved one. Clearly communicate your boundaries and be consistent in enforcing them.
- Connect with support groups: Look for support groups or online communities that cater to individuals with BPD and their loved ones. Connecting with others who are going through similar experiences can provide a sense of validation, understanding, and support for both you and your loved one.
- Practice self-care: Taking care of your own mental and emotional well-being is crucial when supporting someone with BPD. Engage in activities that help you relax, recharge and seek support from friends, family, or a therapist when needed.
Remember that supporting someone with BPD can be challenging at times, but your understanding and support can make a significant difference in their journey towards recovery. Don’t hesitate to reach out for help and to ask for support when you need it.
Resources and Further Reading
There are a range of resources available for individuals seeking help and support for borderline personality disorder. Whether you are looking for therapy, self-help tools, or information on understanding the disorder, the following resources can provide valuable insights:
- National Institute of Mental Health (NIMH) – The NIMH website provides comprehensive information on BPD, including symptoms, treatment options, and research updates. Visit www.nimh.nih.gov for more information.
- Psychology Today – Psychology Today offers a directory of therapists specializing in BPD. You can search for professionals in your area and find therapists who provide the specific treatment approaches you are interested in. Visit www.psychologytoday.com to access the directory.
- Borderline Personality Disorder Resource Center (BPDRC) – BPDRC is an online resource that provides information, articles, and forums for individuals and families affected by BPD. You can find support groups, treatment options, and other resources to help you better understand and manage the disorder. Check out www.borderlinepersonalitydisorder.org for more information.
- Rethink Mental Illness – Rethink Mental Illness is a UK-based charity that provides information, helplines, and support groups for individuals affected by BPD. They offer a range of resources to help individuals better understand and manage the disorder. Visit www.rethink.org to access their resources.
- Books on Borderline Personality Disorder – There are several books available that provide in-depth information on BPD, self-help strategies, and personal stories of individuals living with the disorder. Some recommended titles include “I Hate You, Don’t Leave Me” by Jerold J. Kreisman and Hal Straus, “Understanding the Borderline Mother” by Christine Ann Lawson, and “Stop Walking on Eggshells” by Paul T. Mason and Randi Kreger.
Remember, seeking support and information is an important step in managing borderline personality disorder. These resources can provide valuable insights and tools to help you on your journey towards recovery.
Questions and answers
What is Borderline Personality Disorder (BPD)?
Borderline Personality Disorder (BPD) is a mental health condition characterized by pervasive instability in relationships, self-image, and emotions. People with BPD often experience intense and unstable relationships, difficulty in regulating emotions, impulsivity, and chronic feelings of emptiness.
What are the symptoms of Borderline Personality Disorder?
The symptoms of Borderline Personality Disorder can vary, but some common symptoms include intense fear of abandonment, a pattern of unstable relationships, self-damaging behaviors such as self-harm or suicidal thoughts, rapid mood swings, chronic feelings of emptiness, and difficulty controlling anger.
How can Borderline Personality Disorder be diagnosed?
Borderline Personality Disorder can be diagnosed by a mental health professional through a thorough evaluation of symptoms and medical history. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides criteria for the diagnosis of BPD, including unstable relationships, identity disturbance, impulsive behavior, and emotional instability.
What are the treatment options for Borderline Personality Disorder?
Treatment options for Borderline Personality Disorder may include therapy, medication, and self-help strategies. Psychotherapy, such as dialectical behavior therapy (DBT) and cognitive-behavioral therapy (CBT), can help individuals with BPD learn skills to manage emotions and improve relationships. Medications, such as antidepressants or mood stabilizers, may be prescribed to help with specific symptoms. Self-help strategies, such as maintaining a healthy lifestyle and practicing self-care, can also be beneficial.
Is there a cure for Borderline Personality Disorder?
There is no known cure for Borderline Personality Disorder, but with proper treatment and support, individuals with BPD can experience significant improvement in symptoms and overall functioning. It is important to work closely with a mental health professional to develop a personalized treatment plan and access the support needed.