It is not uncommon for individuals with Irritable Bowel Syndrome (IBS) to also experience symptoms of anxiety. In fact, research has shown that there is a strong connection between the two, with many individuals reporting that their anxiety symptoms worsen when their IBS symptoms flare up.
IBS is a disorder that affects the digestive system and is characterized by symptoms such as abdominal pain, bloating, constipation, and diarrhea. These symptoms can be both physically and emotionally distressing, leading to increased levels of anxiety. Similarly, anxiety can also have a negative impact on the digestive system, potentially exacerbating IBS symptoms.
The exact cause of the link between IBS and anxiety is not yet fully understood, but there are several theories. One theory suggests that the brain-gut axis, which is the bidirectional communication pathway between the brain and the gut, plays a role in the development and exacerbation of both IBS and anxiety symptoms. Another theory proposes that individuals with IBS may have heightened sensitivity to intestinal pain, which can lead to increased levels of anxiety.
Understanding the connection between IBS and anxiety is important for both individuals with these conditions and healthcare professionals. By recognizing and addressing the link, it may be possible to develop more effective treatment strategies that target both the digestive and emotional aspects of these disorders. Additionally, individuals with IBS and anxiety can benefit from learning coping techniques and stress management strategies to help alleviate symptoms and improve overall quality of life.
What is Irritable Bowel Syndrome (IBS)?
Irritable Bowel Syndrome (IBS) is a common digestive disorder that affects the large intestine, also known as the colon. It is characterized by a combination of symptoms such as abdominal pain, bloating, constipation, and diarrhea. The exact cause of IBS is unknown, but it is believed to be a result of a combination of factors including abnormal muscle contractions in the colon, heightened sensitivity to pain, and changes in the gut bacteria.
IBS is a chronic condition that can be difficult to manage, as the symptoms can vary from person to person and may come and go over time. It is estimated that about 10-15% of the global population is affected by IBS, with women being more commonly affected than men.
The exact cause of IBS is still not fully understood, but researchers believe that a combination of factors contributes to its development. These factors may include:
- Abnormal muscle contractions: The muscles in the colon may contract too strongly, leading to cramping and diarrhea, or too weakly, leading to constipation.
- Nervous system abnormalities: People with IBS may have an increased sensitivity to pain and a heightened response to stress, which can affect the functioning of the digestive system.
- Changes in gut bacteria: The balance of bacteria in the gut may be altered in individuals with IBS, leading to symptoms.
- Food sensitivities: Certain foods or drinks, such as dairy products, caffeine, or alcohol, may trigger symptoms in some individuals.
Diagnosing IBS involves ruling out other conditions with similar symptoms through various tests, such as a physical examination, blood tests, stool tests, and imaging tests. While there is no cure for IBS, treatment focuses on managing symptoms and reducing triggers. This may include dietary changes, medications to relieve symptoms, stress management techniques, and lifestyle modifications.
| Common Symptoms of IBS |
|---|
| Abdominal pain and cramping |
| Bloating and gas |
| Diarrhea |
| Constipation |
| Alternating bouts of diarrhea and constipation |
What is Anxiety?
Anxiety is a common mental health condition that is characterized by feelings of worry, fear, and unease. It is a normal and natural response to stress or danger, but for some individuals, it becomes excessive and can interfere with daily life.
Some common symptoms of anxiety include:
- Excessive worrying: Constant worry or fear about everyday situations, even when there is no apparent reason for concern.
- Restlessness: Feeling on edge, unable to relax, or having difficulty concentrating.
- Irritability: Easily becoming irritated or agitated over small things.
- Panic attacks: Sudden episodes of intense fear or physical discomfort, such as rapid heartbeat, shortness of breath, or dizziness.
- Sleep problems: Difficulty falling asleep, staying asleep, or having restless and unsatisfying sleep.
- Physical symptoms: Anxiety can also cause physical symptoms such as headaches, muscle tension, stomachaches, and fatigue.
It is important to note that anxiety can manifest differently in different individuals, and not everyone will experience the same symptoms or to the same degree.
Anxiety can be caused by a variety of factors, including genetic predisposition, brain chemistry, personality traits, traumatic events, and ongoing stress. It can also be a symptom of certain medical conditions or a side effect of medication.
When anxiety becomes chronic or severe, it can significantly impact a person’s quality of life and overall well-being. It can affect their ability to work or go to school, maintain relationships, and engage in everyday activities.
It is crucial to seek professional help if you believe you may be experiencing anxiety. A mental health professional can provide an accurate diagnosis and recommend appropriate treatment, which may include therapy, medication, or a combination of both.
The Prevalence of IBS and Anxiety
Irritable bowel syndrome (IBS) and anxiety are both common health conditions that can significantly impact a person’s quality of life. It is not uncommon for individuals with IBS to also experience symptoms of anxiety, and research has established a strong connection between the two.
IBS affects an estimated 10-15% of the global population, making it one of the most prevalent gastrointestinal disorders. It is characterized by recurring abdominal pain, bloating, gas, diarrhea, and/or constipation. IBS is a chronic condition, and while the exact cause is unknown, it is believed to involve a combination of genetic, environmental, and psychological factors.
Anxiety is a mental health disorder characterized by excessive worry, fear, and apprehension. It is known to affect over 284 million people globally, making it one of the most common mental health conditions. Anxiety can manifest in various forms, such as generalized anxiety disorder (GAD), panic disorder, social anxiety disorder, and post-traumatic stress disorder (PTSD).
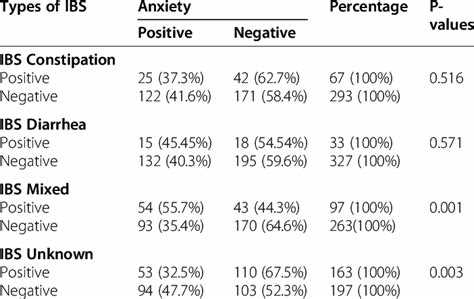
Studies have shown that there is a high comorbidity (co-occurrence) between IBS and anxiety. Research conducted on large populations has found that individuals with IBS are approximately 2-3 times more likely to have anxiety compared to those without IBS. Similarly, individuals with anxiety are also more likely to develop IBS. The relationship between IBS and anxiety is bi-directional, meaning that they can exacerbate each other.
One possible explanation for the co-occurrence of IBS and anxiety is the gut-brain axis. This bidirectional communication system between the gut and the brain involves multiple pathways, including the immune system, nerves, hormones, and neurotransmitters. Dysfunction in the gut-brain axis may contribute to both IBS and anxiety symptoms.
The exact mechanisms by which IBS and anxiety are linked are still being researched. However, it is believed that factors such as heightened stress response, altered intestinal motility, gut dysbiosis (imbalanced gut microbiota), and abnormal serotonin signaling may play a role.
Understanding the connection between IBS and anxiety is important for both healthcare providers and individuals affected by these conditions. Addressing symptoms of anxiety may help improve IBS symptoms, and vice versa. A multidisciplinary approach that combines psychological interventions, dietary modifications, and medical treatments may be beneficial in managing both IBS and anxiety.
In conclusion, IBS and anxiety are prevalent conditions that often co-occur. The connection between the two is complex and involves various physiological and psychological factors. By recognizing and addressing this link, healthcare professionals can provide more comprehensive care for individuals with IBS and anxiety, leading to improved quality of life.
The Link Between IBS and Anxiety
There is a strong connection between Irritable Bowel Syndrome (IBS) and anxiety. Many individuals who suffer from IBS also experience symptoms of anxiety, and vice versa. Understanding this link is crucial for effective treatment and management of both conditions.
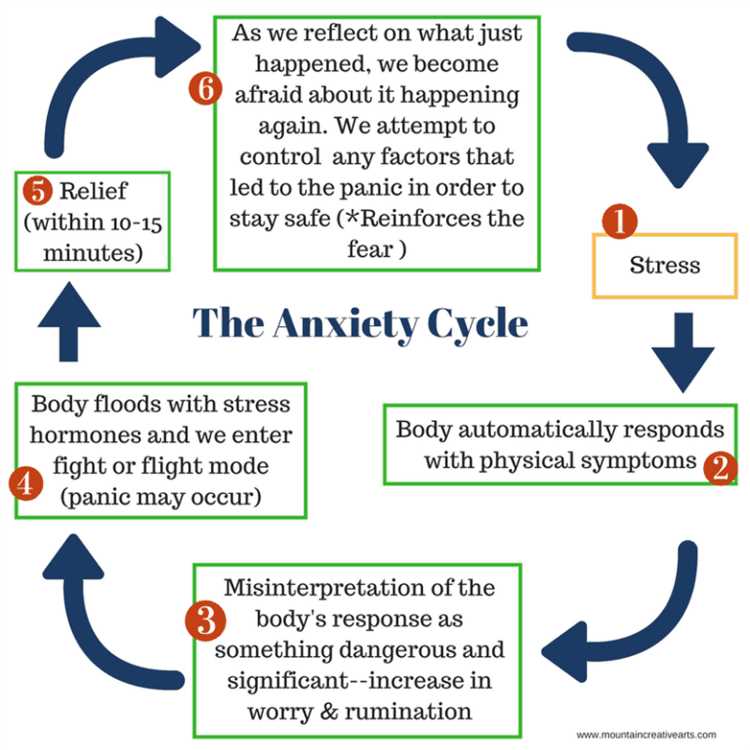
1. Stress and Anxiety
Stress and anxiety can trigger IBS symptoms or exacerbate existing ones. When you are under stress, your body releases stress hormones that can affect the functioning of your digestive system. This can lead to symptoms such as abdominal pain, diarrhea, or constipation, which are commonly associated with IBS.
2. Gut-Brain Axis
The gut-brain axis refers to the bidirectional communication between the gut and the brain. The gut has its own nervous system, known as the enteric nervous system, which communicates with the central nervous system. This communication plays a role in regulating gut function and can be disrupted in individuals with IBS and anxiety.
3. Shared Pathways
IBS and anxiety share common pathways in the brain. Serotonin, a neurotransmitter involved in regulating mood, is found in high concentrations in the gut. When the levels of serotonin in the brain and gut are imbalanced, it can result in both IBS and anxiety symptoms.
4. Psychological Factors
Psychological factors, such as a history of trauma or a tendency towards perfectionism, can contribute to both IBS and anxiety. These factors can influence the way an individual processes stress and can increase the likelihood of developing both conditions.
5. Treatment Approaches
Considering the link between IBS and anxiety, treatment approaches should address both conditions. This may include a combination of lifestyle changes, stress management techniques, psychological therapy, and medications to target symptoms of both IBS and anxiety.
| Triggers: | Stress and anxiety |
| Gut-Brain Axis: | Communication between gut and brain |
| Shared Pathways: | Imbalanced serotonin levels |
| Psychological Factors: | History of trauma, perfectionism |
| Treatment Approaches: | Lifestyle changes, stress management, therapy, medications |
In conclusion, the link between IBS and anxiety is significant. By addressing both conditions together, individuals can better manage their symptoms and improve their overall quality of life.
The Role of Stress in IBS and Anxiety
Stress plays a significant role in both irritable bowel syndrome (IBS) and anxiety. While the exact relationship between the two conditions is complex and not fully understood, several factors contribute to their interconnectedness.
1. Brain-Gut Axis: The brain-gut axis is the communication network between the brain and the gut. Stress can disrupt the normal functioning of this axis, leading to changes in gut motility, sensitivity, and function. Consequently, stress can trigger or exacerbate IBS symptoms, such as abdominal pain, bloating, and bowel irregularities.
2. Increased Sensitivity: Stress activates the body’s stress response system, releasing hormones like cortisol and adrenaline. These hormones can heighten sensation and increase the perception of pain in the gut. People with IBS often have hyperactive sensory nerves in their intestines, making them more susceptible to experiencing pain and discomfort in response to stress.
3. Altered Gut Microbiota: Chronic stress can disrupt the composition and diversity of gut microbiota – the trillions of microorganisms that reside in the digestive tract. This disturbance in the gut microbial balance can contribute to gastrointestinal symptoms and may also impact mental health. Emerging research suggests that imbalances in the gut microbiota play a role in the development and maintenance of anxiety disorders.
4. Psychological Factors: The distress caused by living with IBS can lead to anxiety and other psychological symptoms. Frequent bowel disruptions, embarrassment, and the constant need to be near a bathroom can significantly impact a person’s quality of life and contribute to feelings of anxiety and stress.
Managing Stress for IBS and Anxiety:
- Stress reduction techniques: Incorporating stress reduction techniques such as deep breathing exercises, meditation, yoga, or tai chi can help alleviate stress and promote a sense of calm.
- Regular exercise: Engaging in regular physical activity can help reduce stress and improve overall well-being.
- Healthy lifestyle: Maintaining a healthy diet, getting enough sleep, and avoiding excessive alcohol and caffeine can also contribute to stress reduction.
- Talk therapy: Working with a therapist or counselor can provide coping strategies for managing stress and anxiety related to IBS.
Understanding the role of stress in IBS and anxiety is crucial in developing effective treatment approaches and improving outcomes for individuals living with these conditions. By addressing stress and its impact on the gut-brain connection, healthcare professionals can support patients in managing their symptoms and improving their overall quality of life.
Managing IBS and Anxiety
1. Recognize the relationship: Understanding the connection between IBS and anxiety is crucial in managing the symptoms of both conditions. Recognize that anxiety can worsen IBS symptoms and vice versa.
2. Seek professional help: Consult a healthcare professional, such as a gastroenterologist or a psychiatrist, who can help diagnose your specific case and develop an appropriate treatment plan.
3. Practice stress management techniques: Stress can trigger IBS symptoms and worsen anxiety. Incorporate stress-reducing activities into your daily routine, such as exercise, deep breathing exercises, meditation, or yoga.
4. Maintain a healthy diet: Make dietary changes to manage IBS symptoms. Consider a low FODMAP diet, which eliminates certain types of carbohydrates that can worsen IBS symptoms. Also, ensure a balanced intake of fiber and hydrate adequately.
5. Regular exercise: Engaging in regular physical activity can help reduce anxiety and improve digestion. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
6. Get enough sleep: Lack of sleep can worsen both IBS and anxiety symptoms. Establish a regular sleep routine and create a comfortable sleep environment to ensure quality rest.
7. Support network: Surround yourself with a supportive network of friends and family who can provide emotional support. Consider joining a support group for individuals with IBS and anxiety to connect with others who understand your experiences.
8. Medications: Depending on the severity of symptoms, your healthcare provider may prescribe medications to manage IBS and anxiety. These may include anti-anxiety medications, antidepressants, or medications specifically designed to treat IBS symptoms.
9. Cognitive-behavioral therapy (CBT): CBT is a type of therapy that can help individuals manage both IBS and anxiety. It focuses on identifying and modifying negative thoughts and behaviors that contribute to these conditions.
10. Monitor and track symptoms: Keep a journal to track your symptoms, including triggers for both IBS and anxiety. This can help you identify patterns and make necessary adjustments to your management plan.
11. Take breaks and relax: Give yourself breaks throughout the day to relax and decompress. Engage in activities you enjoy and that promote relaxation, such as reading, listening to music, or taking a warm bath.
12. Seek therapy or counseling: If anxiety is significantly impacting your daily life or if you are struggling to manage your IBS symptoms, consider seeing a therapist or counselor who specializes in anxiety disorders and gastrointestinal conditions.
13. Educate yourself: Learn as much as you can about IBS and anxiety. Understanding the conditions and their relationship can empower you to better manage and cope with your symptoms.
Seeking Professional Help for IBS and Anxiety
If you are experiencing symptoms of both IBS and anxiety, it is important to seek professional help. Only a healthcare provider can properly diagnose and treat these conditions. Here are some steps you can take:
- Consult a Doctor: Begin by scheduling an appointment with your primary care physician. They can evaluate your symptoms, provide a proper diagnosis, and recommend appropriate treatment options.
- Consider a Specialist: In some cases, your primary care physician may refer you to a specialist such as a gastroenterologist or a psychiatrist. These doctors have expertise in treating IBS and anxiety, respectively.
- Get a Comprehensive Assessment: During your appointment, your healthcare provider will likely ask you about your medical history, perform a physical examination, and order relevant tests. This will help to rule out any other potential causes of your symptoms.
- Explore Treatment Options: Depending on the severity and impact of your symptoms, your doctor may recommend various treatment modalities. These can include medications, psychological therapies, dietary modifications, and stress-management techniques.
- Follow the Treatment Plan: It is crucial to follow your healthcare provider’s recommendations and treatment plan consistently. This includes taking prescribed medications as directed and attending any therapy sessions or follow-up appointments.
- Consider Support Groups: Joining a support group for individuals with IBS or anxiety can provide additional resources and a community of people who understand what you are going through. Your healthcare provider may be able to recommend local or online support groups.
Remember, seeking professional help is the first step towards managing and finding relief from the symptoms of IBS and anxiety. With the right support and treatment, it is possible to regain control over your physical and mental well-being.
Questions and answers
Can anxiety cause IBS?
Yes, anxiety can contribute to the development of IBS. Studies have shown that there is a strong connection between anxiety and IBS, with anxiety often preceding IBS symptoms. Stress and anxiety can affect the functioning of the digestive system and lead to symptoms such as abdominal pain, bloating, and changes in bowel movements.
How does anxiety affect IBS?
Anxiety can worsen the symptoms of IBS. When a person is anxious, their body releases stress hormones that can trigger changes in the digestive system, leading to increased sensitivity, inflammation, and alterations in bowel movements. Anxiety can also make it harder for individuals with IBS to manage their symptoms effectively.
What are some common symptoms of IBS and anxiety?
Common symptoms of IBS include abdominal pain, bloating, gas, diarrhea or constipation, and changes in bowel movements. Anxiety symptoms can manifest as excessive worry, restlessness, difficulty concentrating, irritability, and physical symptoms like a racing heart or shortness of breath.
How can I manage both my IBS and anxiety?
Managing both IBS and anxiety involves a multi-faceted approach. Strategies may include lifestyle modifications such as practicing stress-reducing techniques like yoga or mindfulness meditation, regular exercise, and maintaining a healthy diet. Seeking therapy or counseling to address anxiety symptoms can also be beneficial. Additionally, certain medications may be prescribed by a healthcare provider to help manage symptoms.