Endometriosis is a condition that affects millions of women around the world. It occurs when the tissue that normally lines the uterus begins to grow outside of it, causing pain and other symptoms. This condition can be challenging to diagnose and manage, but with the right information and treatment options, women with endometriosis can find relief and improve their quality of life.
The exact cause of endometriosis is not fully understood, but there are several theories. One possibility is that during menstruation, some of the tissue backs up through the fallopian tubes and attaches to the pelvic walls and organs. Another theory suggests that endometrial cells are distributed throughout the body via the bloodstream or lymphatic system.
Some common symptoms of endometriosis include pelvic pain, painful periods, pain during intercourse, and infertility. Additionally, women with endometriosis may experience heavy or irregular periods, fatigue, and bowel or bladder problems. It’s important to note that not all women with endometriosis will have all of these symptoms, and the severity can vary from person to person.
While there is currently no cure for endometriosis, there are various treatment options available to manage the symptoms and improve quality of life. These may include pain medication, hormonal therapies, and surgery. The specific treatment approach will depend on factors such as the severity of symptoms, a woman’s desire to conceive, and her overall health. It’s important for women to work closely with their healthcare provider to develop a personalized treatment plan.
In conclusion, endometriosis is a complex condition that can have a significant impact on a woman’s life. By understanding the causes, symptoms, and treatment options available, women with endometriosis can better manage their condition and improve their overall well-being.
The Basics of Endometriosis
Endometriosis is a condition that occurs when the tissue that lines the uterus, called the endometrium, starts growing outside the uterus. This abnormal growth can occur in various areas of the body, including the ovaries, fallopian tubes, and the tissue lining the pelvis.
Common symptoms of endometriosis include:
- Severe menstrual cramps
- Chronic pelvic pain
- Heavy or irregular periods
- Pain during intercourse
- Infertility
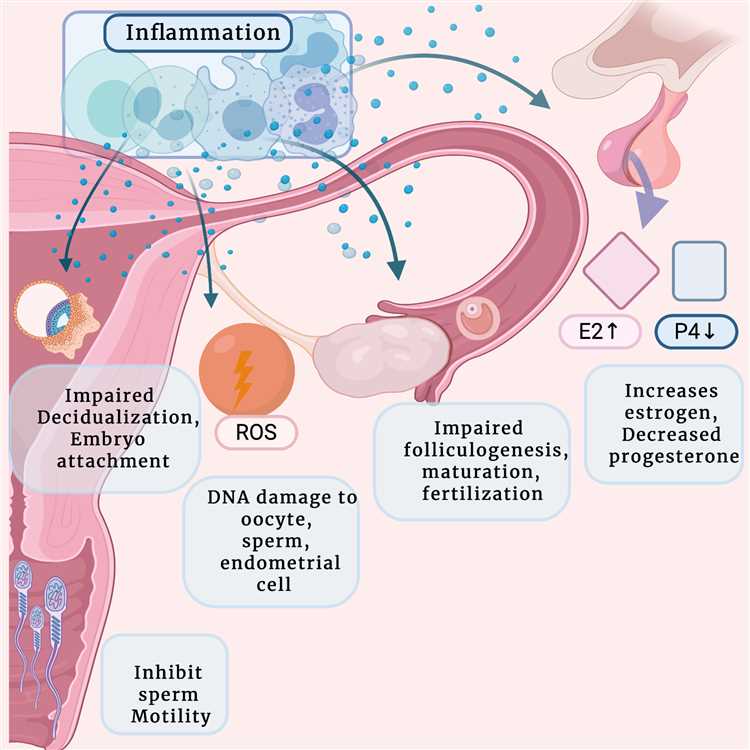
It is estimated that over 176 million women worldwide have endometriosis. The exact cause of endometriosis is unknown, but there are several theories. One theory suggests that endometriosis may occur when cells from the endometrium travel backward through the fallopian tubes and implant in the pelvis. Another theory suggests that it may be a result of a faulty immune system, which allows the endometrial tissue to grow outside the uterus.
Diagnosing endometriosis can be challenging because its symptoms can be similar to other conditions. However, the gold standard for diagnosing endometriosis is through laparoscopic surgery, where a thin tube with a camera is inserted into the abdomen to visualize the pelvic organs and detect any abnormal growth of endometrial tissue.
There is currently no cure for endometriosis, but there are treatment options available to manage the symptoms and improve quality of life. Treatment may include pain medication, hormone therapy, or surgery to remove the abnormal tissue.
It is important for women who suspect they may have endometriosis to consult with a healthcare professional for proper diagnosis and treatment. Early detection and management of endometriosis can help prevent complications and improve overall health and well-being.
Common Causes of Endometriosis
Endometriosis is a gynecological condition where the tissue that normally lines the inside of the uterus, called the endometrium, grows outside of the uterus. While the exact cause of endometriosis is still unknown, there are several theories regarding its development.
1. Retrograde Menstruation: One theory suggests that endometriosis occurs when menstrual blood containing endometrial cells flows back through the fallopian tubes into the pelvic cavity instead of leaving the body. These cells then implant and grow in different areas outside the uterus.
2. Genetic Factors: There is evidence to suggest that endometriosis may have a hereditary component. If a close family member, such as a mother or sister, has endometriosis, the risk of developing the condition may be higher.
3. Hormonal Imbalances: Hormones play a crucial role in the development and progression of endometriosis. An imbalance in hormone levels, particularly estrogen, may contribute to the growth and development of endometrial tissue outside the uterus.
4. Immune System Dysfunction: Some researchers believe that problems with the immune system may contribute to the development of endometriosis. An impaired immune response may allow endometrial cells to implant and grow in abnormal locations in the body.
5. Environmental Factors: Exposure to certain environmental factors, such as chemicals or toxins, may increase the risk of developing endometriosis. However, more research is needed to understand the direct impact of these factors on the development of the condition.
6. Surgical Scar Implantation: Scar tissue from previous surgeries, such as cesarean sections or hysterectomies, may provide a site for the implantation and growth of endometrial cells.
7. Autoimmune Response: Another theory suggests that endometriosis may result from an autoimmune response, where the immune system mistakenly attacks the body’s own tissues, including the endometrial tissue.
It’s important to note that these theories are not mutually exclusive, and it’s likely that multiple factors contribute to the development of endometriosis in different individuals. Medical professionals continue to conduct research to better understand the causes of endometriosis and develop more effective treatment options.
Recognizing the Symptoms of Endometriosis
Endometriosis is a condition in which the tissue that lines the uterus begins to grow outside of the uterus, leading to a range of symptoms. Recognizing the symptoms of endometriosis is crucial for early detection and treatment.
Common Symptoms
- Painful periods (dysmenorrhea): Severe menstrual cramps that may worsen over time
- Chronic pelvic pain: Constant pain in the pelvic region outside of menstruation
- Painful intercourse (dyspareunia): Pain during or after sexual intercourse
- Heavy or irregular periods: Menstrual bleeding that is significantly heavier or lasts longer than usual
- Infertility: Difficulty getting pregnant or conceiving
Other Possible Symptoms
- Bowel or urinary problems: Painful bowel movements, constipation, diarrhea, or pain during urination
- Chronic fatigue: Feeling tired or exhausted on a regular basis
- Digestive issues: Bloating, nausea, or gastrointestinal discomfort
- Painful bowel movements: Pain during bowel movements or blood in the stool
- Back or leg pain: Pain in the lower back or legs, especially during menstruation
When to See a Doctor
If you experience any of the symptoms mentioned above, it is important to consult a healthcare provider. While these symptoms can be caused by other conditions, a doctor can evaluate your symptoms, perform necessary tests, and provide an accurate diagnosis. Early diagnosis and treatment can help manage the symptoms and prevent further complications.
Diagnosing Endometriosis
Diagnosing endometriosis can be challenging as its symptoms can vary and be similar to other conditions. However, there are several diagnostic tools that healthcare providers use to determine if a person has endometriosis.
1. Medical History: A doctor will start by taking a detailed medical history, including asking about symptoms, menstrual cycle patterns, and any previous surgeries or conditions that may be related.
2. Physical Exam: A pelvic exam may be performed to check for any abnormalities, such as the presence of cysts or scars that may indicate endometriosis.
3. Imaging Tests: In some cases, imaging tests such as ultrasound or MRI may be used to detect the presence of endometriosis. These tests can help visualize the pelvic region and identify any abnormalities.
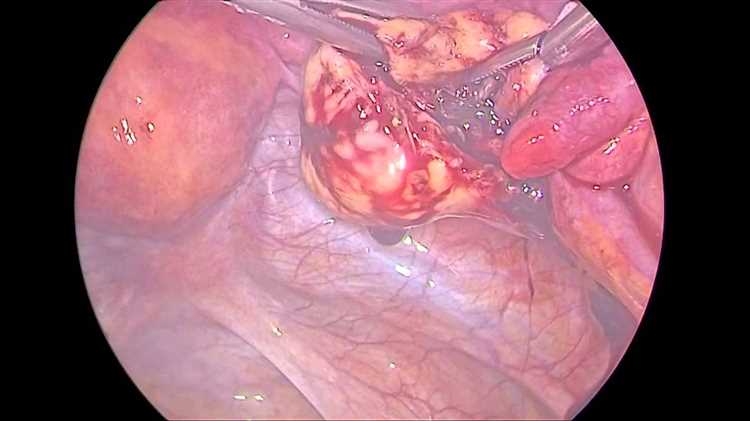
4. Laparoscopy: Laparoscopy is the most common and definitive method to diagnose endometriosis. It is a minimally invasive surgical procedure where a thin tube with a camera is inserted through a small incision in the abdomen. This allows the doctor to directly visualize and biopsy any abnormal tissue or lesions.
5. Biopsy: During laparoscopy, the doctor may take a small tissue sample (biopsy) for further examination in a laboratory. This can help confirm the presence of endometriosis and determine its severity.
6. Pain Mapping: Some healthcare providers may use a technique called pain mapping to identify and localize specific areas of pain in the pelvis. This can help guide treatment and better understand the extent of endometriosis.
It is important to note that diagnosing endometriosis may require a combination of these diagnostic tools and that the definitive diagnosis can only be made through laparoscopy and biopsy.
If you suspect that you may have endometriosis, it is crucial to consult with a healthcare provider who specializes in reproductive health or gynecology. They can evaluate your symptoms, perform the necessary tests, and provide appropriate treatment options.
Available Treatment Options for Endometriosis
Endometriosis is a condition in which the tissue that lines the uterus grows outside of the uterus. It can cause severe pain and discomfort, as well as other symptoms such as irregular bleeding and infertility. While there is no known cure for endometriosis, there are several treatment options available to help manage the symptoms and improve quality of life for those affected.
1. Pain Medication
Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate the pain associated with endometriosis. Prescription pain medication may be necessary for more severe cases.
2. Hormonal Therapy
Hormonal therapy is a common treatment option for endometriosis. This can include birth control pills, which help regulate hormone levels and reduce the growth of endometrial tissue. Other hormonal therapies, such as gonadotropin-releasing hormone agonists or antagonists, may be prescribed to stop the production of estrogen and induce a temporary menopause-like state.
3. Laparoscopic Surgery
Laparoscopic surgery is often recommended for women with severe symptoms or who do not respond well to other treatments. During this minimally invasive procedure, a surgeon makes small incisions in the abdomen and inserts a laparoscope to remove or destroy abnormal tissue.
4. Hysterectomy
In cases where other treatments have been ineffective or the endometriosis is severe, a hysterectomy may be considered. This surgical procedure involves removing the uterus and, in some cases, the ovaries. It is important to note that a hysterectomy is not a cure for endometriosis and should only be considered as a last resort.
5. Alternative Therapies
Some individuals with endometriosis find relief from alternative therapies such as acupuncture, chiropractic care, or herbal remedies. While these treatments may not address the underlying cause of endometriosis, they can help manage symptoms and improve overall well-being.
6. Lifestyle Changes
Implementing lifestyle changes, such as maintaining a healthy diet, exercising regularly, and managing stress, can also help alleviate symptoms of endometriosis. Additionally, avoiding known triggers, such as certain foods or environmental toxins, may help reduce the severity of symptoms.
| Pain Medication | Hormonal Therapy | Laparoscopic Surgery | Hysterectomy | Alternative Therapies | Lifestyle Changes | |
|---|---|---|---|---|---|---|
| Effectiveness | ✅ | ✅ | ✅✅ | ✅✅ | ❌ (Varies) | ❌ (Varies) |
| Risks | ❌ (Long-term use) | ❌ (Side effects) | ❌ (Surgical risks) | ✅✅ | ❌ (Varies) | ❌ (None) |
| Cost | ✅ | ✅✅ | ✅✅ (Higher) | ✅✅ (Higher) | ❌ (Varies) | ❌ (Varies) |
| Long-term Impact | ❌ (Dependency) | ❌ (Hormone imbalance) | ❌ (Possible recurrence) | ✅✅ | ❌ (Varies) | ✅✅ |
Note: The effectiveness, risks, cost, and long-term impact may vary depending on the individual and the severity of endometriosis.
It is important to consult with a healthcare professional to discuss the available treatment options and determine the best course of action based on your specific situation. Together, you can create a personalized treatment plan to manage symptoms and improve your quality of life.
Medications for Managing Endometriosis Symptoms
Endometriosis is a chronic condition that affects the lining of the uterus, known as the endometrium. It can cause various symptoms, such as pelvic pain, heavy menstrual bleeding, and fertility issues. While surgery is often recommended for the treatment of endometriosis, medications can also be used to manage the symptoms and reduce the progression of the condition.
1. Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- NSAIDs, such as ibuprofen and naproxen, are commonly used to relieve pain and reduce inflammation associated with endometriosis.
- They work by decreasing prostaglandin production, which is responsible for pain and inflammation.
2. Hormonal Contraceptives
- Birth control pills, patches, and vaginal rings contain hormones that prevent ovulation, reduce hormone fluctuations, and suppress the growth of endometrial tissue.
- These hormonal contraceptives can help relieve pain and regulate periods.
3. Gonadotropin-releasing Hormone (GnRH) Agonists
- GnRH agonists, such as leuprolide and nafarelin, work by suppressing the production of estrogen, which helps to shrink endometrial growths.
- These medications can induce a temporary menopause-like state, which may help relieve symptoms.
4. Progestin Therapy
- Progestins, such as medroxyprogesterone acetate and norethindrone, can help regulate menstrual cycles and reduce the growth of endometrial tissue.
- These medications can be taken orally or administered through injections.
5. Aromatase Inhibitors
- Aromatase inhibitors, such as anastrozole and letrozole, work by blocking the production of estrogen, which can help reduce the growth and spread of endometriosis.
- These medications are typically used in combination with other therapies.
6. Danazol
- Danazol is a synthetic hormone that suppresses the production of estrogen and progesterone, creating a temporary state of pseudo-menopause.
- It can help relieve symptoms and reduce the size of endometrial growths, but it may cause side effects such as weight gain and acne.
7. Pain Medications
- In addition to NSAIDs, pain medications such as opioids and muscle relaxants may be prescribed to manage severe pain associated with endometriosis.
- These medications should be used under the guidance of a healthcare professional, as they can have side effects and may be addictive.
It’s important to note that every individual may respond differently to medications, and a healthcare professional should be consulted for personalized treatment recommendations. Combination therapies, including both medications and surgery, may provide the best outcomes for managing endometriosis symptoms.
Surgical Procedures for Endometriosis Treatment
When conservative treatments fail to provide relief or manage the symptoms of endometriosis, surgical intervention may be necessary. Surgical procedures are often recommended for women with severe endometriosis or when fertility preservation is a concern. The goal of surgery is to remove or destroy the endometrial tissue and alleviate pain.
- Laparoscopy: Laparoscopy is the most common surgical procedure used for the diagnosis and treatment of endometriosis. It involves making small incisions in the abdomen and inserting a thin, lighted tube with a camera (laparoscope) to visualize and access the pelvic organs. During the laparoscopy, the surgeon can remove the endometrial growths, cysts, scar tissue, or adhesions. This minimally invasive procedure offers faster recovery times and less scarring compared to traditional open surgery.
- Laparotomy: Laparotomy is a more invasive surgical procedure that involves making a larger incision in the abdomen to access the pelvic organs. It is typically reserved for severe cases of endometriosis or when laparoscopy is not feasible. Laparotomy allows the surgeon to thoroughly examine and treat the affected areas, remove large growths or cysts, and repair any organ damage. It is often performed when fertility preservation is a primary concern.
- Hysterectomy: In cases where endometriosis is extensive and causing debilitating pain that does not respond to other treatments, a hysterectomy may be considered. A hysterectomy involves surgical removal of the uterus and sometimes the ovaries and fallopian tubes. This procedure effectively eliminates menstruation and can provide long-term relief from endometriosis symptoms. However, it is only recommended as a last resort and may not be suitable for women who desire to have children in the future.
It is important to discuss the available surgical options with a healthcare provider specialized in endometriosis treatment. The choice of surgery will depend on the severity of endometriosis, individual symptoms, and the patient’s fertility goals. Surgery for endometriosis should always be performed by a skilled surgeon experienced in treating the condition to ensure optimal outcomes and minimize potential complications.
Lifestyle Changes to Help Manage Endometriosis
If you have been diagnosed with endometriosis, there are several lifestyle changes you can make to help manage your symptoms and improve your overall quality of life. While these changes may not eliminate the condition entirely, they can provide relief and reduce the impact endometriosis has on your daily life.
1. Diet
Adopting a healthy, balanced diet can support your overall well-being and potentially alleviate endometriosis symptoms. Focus on incorporating fresh fruits and vegetables, whole grains, lean proteins, and healthy fats into your meals. Avoiding processed foods, excessive sugar, caffeine, and alcohol may also be beneficial.
2. Exercise
Regular exercise can help reduce pain, manage stress, and support a healthy weight. Engaging in activities such as walking, swimming, yoga, or low-impact aerobics can be beneficial for women with endometriosis. It’s important to consult with your healthcare provider to determine the appropriate level of exercise for your condition.
3. Stress Management
Stress can exacerbate endometriosis symptoms, so finding effective ways to manage stress is crucial. Consider incorporating stress-reducing techniques into your daily routine, such as meditation, deep breathing exercises, yoga, or engaging in hobbies that bring you joy.
4. Sleep
Prioritizing quality sleep can help improve overall well-being and reduce pain associated with endometriosis. Establish a regular sleep routine and create a comfortable sleep environment that promotes relaxation.
5. Natural Remedies
Some women find relief from endometriosis symptoms by incorporating natural remedies into their treatment plan. These can include herbal supplements (e.g., turmeric, ginger), acupuncture, or chiropractic care. Before trying any natural remedies, it’s important to consult with your healthcare provider.
6. Support Network
Building a support network of friends, family, or joining a support group can provide emotional support and helpful resources for managing endometriosis. Sharing your experiences and connecting with others who understand what you’re going through can be incredibly beneficial.
7. Communication
Openly communicate with your healthcare provider about your symptoms, concerns, and treatment options. Working together to develop a personalized management plan can help ensure you receive the best care possible.
It’s important to remember that each woman’s experience with endometriosis is unique, and what works for one person may not work for another. Experiment with different lifestyle changes and treatments to find what helps alleviate your symptoms and improves your quality of life.
Questions and answers
What is endometriosis?
Endometriosis is a medical condition in which the tissue that normally lines the inside of the uterus, called the endometrium, grows outside the uterus.
What causes endometriosis?
The exact cause of endometriosis is unknown, but there are several theories. One theory suggests that endometrial tissue may flow back through the fallopian tubes into the pelvic cavity during menstruation, while another theory suggests that certain cells in the pelvic lining may transform into endometrial cells.
What are the symptoms of endometriosis?
The symptoms of endometriosis can vary, but common symptoms include pelvic pain, painful periods, heavy menstrual bleeding, pain during sex, and infertility. Some women may also experience fatigue, diarrhea, constipation, and bloating.
How is endometriosis treated?
Treatment for endometriosis may include pain medication, hormonal therapy, and surgery. Pain medication can help manage the pain associated with endometriosis, while hormonal therapy, such as birth control pills or gonadotropin-releasing hormone agonists, can help regulate hormone levels and reduce symptoms. In severe cases, surgery may be necessary to remove endometrial tissue or repair any damage caused by the condition.