Obsessive Compulsive Disorder (OCD) is a chronic mental health condition that affects millions of people worldwide. It is characterized by intrusive thoughts and repetitive behaviors that individuals find difficult to control. These obsessions and compulsions can significantly impact a person’s daily life, causing distress and interfering with their ability to function effectively.
The exact cause of OCD is still unknown, but it is believed to be a combination of genetic, neurological, and environmental factors. Studies have shown that individuals with a family history of OCD are more likely to develop the disorder themselves. Moreover, imbalances in certain brain chemicals, such as serotonin, have been associated with the development of OCD. Additionally, traumatic life events or high levels of stress can trigger or exacerbate symptoms.
The symptoms of OCD can vary from person to person, but commonly include recurring thoughts or images that cause anxiety or distress, and a deep-seated urge to perform certain rituals or actions to alleviate this anxiety. These rituals, or compulsions, are often time-consuming and can interfere with daily functioning. Examples include excessive cleaning or checking, arranging objects in a specific order, or repeating certain phrases or prayers.
Treatment for OCD typically involves a combination of therapy and medication. Cognitive Behavioral Therapy (CBT) is commonly used to help individuals understand and challenge their irrational thoughts and develop healthier coping mechanisms. Medications, such as selective serotonin reuptake inhibitors (SSRIs), may also be prescribed to help regulate brain chemistry and reduce symptoms. In severe cases, when other treatments have been ineffective, deep brain stimulation may be considered as a last resort.
In conclusion,Obsessive Compulsive Disorder is a complex mental health condition that can significantly impact a person’s life. While the exact cause is still unknown, a combination of genetic, neurological, and environmental factors is believed to play a role. Understanding the causes, symptoms, and treatment options for OCD is crucial in order to provide individuals with the necessary support and help them manage their condition effectively.
Understanding Obsessive Compulsive Disorder
Obsessive Compulsive Disorder (OCD) is a mental health disorder characterized by recurring, intrusive thoughts (obsessions) and the need to perform certain repetitive behaviors (compulsions) in order to alleviate anxiety or distress. It affects millions of people worldwide and can significantly interfere with daily life.
Causes of OCD:
- Genetics: Studies have shown that OCD has a genetic component, with certain genes being linked to an increased risk of developing the disorder.
- Brain chemistry and structure: Imbalances in neurotransmitters such as serotonin may play a role in the development of OCD. Differences in brain structure and functioning have also been observed in individuals with OCD.
- Environmental factors: Traumatic events, such as physical or sexual abuse, can trigger the onset of OCD in some individuals, while others may develop OCD as a way to cope with stress or anxiety.
Symptoms of OCD:
- Obsessions: Persistent, unwanted thoughts, images, or urges that cause significant distress. Common obsessions include contamination fears, concerns about symmetry or orderliness, and intrusive thoughts of violence or harm.
- Compulsions: Repetitive behaviors or mental acts performed in response to obsessions. These actions are often aimed at reducing anxiety or preventing a feared event. Examples of compulsions include excessive handwashing, checking and re-checking, and counting or arranging objects in specific ways.
- Anxiety and distress: The obsessions and compulsions of OCD can cause intense anxiety and distress, leading to significant impairment in social, occupational, and academic functioning.
Treatment of OCD:
OCD is a treatable condition, and several approaches can be effective in managing symptoms:
- Cognitive Behavioral Therapy (CBT): This therapy aims to help individuals identify and challenge their obsessive thoughts and develop healthier coping strategies. Exposure and response prevention (ERP) is a specific type of CBT that gradually exposes individuals to their fears and prevents the accompanying compulsions.
- Medication: Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to reduce the symptoms of OCD. These medications work by increasing the availability of serotonin in the brain.
- Support groups: Joining a support group with others who have OCD can provide a sense of community and understanding, as well as the opportunity to share experiences and coping strategies.
It’s important to remember that OCD is a medical condition and not a personal failure or weakness. With the right treatment and support, individuals with OCD can lead fulfilling lives and manage their symptoms effectively.
Causes of Obsessive Compulsive Disorder
Obsessive Compulsive Disorder (OCD) is a complex mental health condition that can be caused by a combination of factors. While the exact cause of OCD is not fully understood, researchers believe that genetics, brain structure and function, and environmental factors play a role in the development of the disorder.
Genetics: There is evidence to suggest that OCD may be hereditary, meaning it can be passed down from parents to their children. Studies have shown that individuals with a family history of OCD are more likely to develop the disorder themselves. However, it is important to note that not everyone with a family history of OCD will develop the condition, and not everyone with OCD has a family history of the disorder.
Brain Structure and Function: Research has also found that individuals with OCD may have differences in their brain structure and function. Specifically, there may be abnormalities in certain areas of the brain, such as the orbitofrontal cortex, anterior cingulate cortex, and basal ganglia, which are involved in the regulation of emotions, decision-making, and behavior. These abnormalities may contribute to the development of obsessive thoughts and compulsive behaviors seen in OCD.
Environmental Factors: In addition to genetic and brain factors, environmental factors may also contribute to the development of OCD. Traumatic events, such as abuse or neglect, can increase the risk of developing the disorder. Stressful life events, such as a major life change or loss, may also trigger symptoms of OCD in individuals who are predisposed to the disorder.
It is important to note that OCD is a complex condition and is likely caused by a combination of these factors. Further research is needed to fully understand the causes of OCD and develop more effective treatments for individuals with the disorder.
Common Symptoms of Obsessive Compulsive Disorder
Obsessive Compulsive Disorder (OCD) is a mental health disorder that affects millions of people worldwide. It is characterized by recurrent and intrusive thoughts, also known as obsessions, and repetitive behaviors, also known as compulsions. OCD can significantly impact a person’s daily life and functioning. Here are some common symptoms of OCD:
- Obsessions: These are persistent, unwanted, and intrusive thoughts, images, or urges that cause distress. Common obsessions include fears of contamination, doubts about safety, a need for symmetry or exactness, and aggressive, sexual, or religious thoughts.
- Compulsions: These are repetitive behaviors or mental acts that individuals with OCD feel driven to perform in response to their obsessions. Common compulsions include excessive cleaning or handwashing, counting or repeating words, checking doors or appliances repeatedly, and arranging objects in a specific order.
- Anxiety: People with OCD often experience high levels of anxiety and distress due to their obsessions and compulsions. The anxiety can be overwhelming and interfere with their ability to carry out daily activities.
- Perfectionism: Individuals with OCD tend to have a strong need for things to be perfect or symmetrical. They may spend excessive amounts of time on tasks to ensure everything is just right.
- Avoidance: Some people with OCD may try to avoid situations or triggers that worsen their obsessions or provoke anxiety. This avoidance can lead to social isolation and difficulty in participating in normal activities.
- Interference in daily life: OCD can significantly impact a person’s daily life, including their relationships, work or school performance, and overall quality of life. The obsessions and compulsions can consume a significant amount of time and energy.
If you or someone you know is experiencing these symptoms, it is essential to seek help from a mental health professional. With proper diagnosis and treatment, individuals with OCD can manage their symptoms and improve their quality of life.
Types of Obsessions and Compulsions
Obsessive Compulsive Disorder (OCD) is a mental health condition characterized by intrusive thoughts and repetitive behaviors. These thoughts are known as obsessions, and the behaviors are referred to as compulsions. OCD can manifest in a variety of ways, and individuals may experience different types of obsessions and compulsions. Here are some common types:
Intrusive Thoughts
One common type of obsession in OCD is intrusive thoughts. These are unwanted and distressing thoughts or images that repeatedly enter a person’s mind. Examples of intrusive thoughts include thoughts of harming oneself or others, thoughts of engaging in sexually inappropriate or violent behaviors, or thoughts about contamination or germs.
Fear of Contamination
Some individuals with OCD have an intense fear of contamination. This fear may be related to germs, chemicals, or dirt. They may excessively wash their hands, clean their belongings, or avoid situations or places they perceive as dirty or contaminated.
Symmetry and Orderliness
Another common obsession in OCD is the need for symmetry and orderliness. People with this type of OCD may feel a strong urge to arrange objects in a specific way or to perform tasks in a specific order. They may spend excessive amounts of time organizing and rearranging items to achieve a sense of balance and symmetry.
Hoarding
Hoarding is a specific type of obsession in which individuals have difficulty discarding or parting with belongings. They may accumulate an excessive amount of items, which can lead to clutter and an inability to use their living space effectively. Hoarding can severely impact a person’s quality of life and functioning.
Checking
Individuals with OCD may also experience compulsions related to checking. They may feel compelled to repeatedly check if the door is locked, the stove is off, or if they have completed a task correctly. This behavior is driven by a fear of something bad happening if they do not check, even if they logically know there is no real danger.
Repeating
Some individuals with OCD have a compulsion to repeat certain actions or behaviors. These repetitions may include actions such as touching objects a certain number of times, repeating words or phrases, or rereading sentences or paragraphs. This compulsion is often driven by a need to prevent something bad from happening.
Counting
Counting is another common compulsion in OCD. Individuals may feel the need to count certain objects or perform actions a specific number of times. This compulsion is often associated with a desire for order and control.
Magical Thinking
Magical thinking is a type of obsession in which individuals believe that their thoughts or actions can influence events in unrealistic ways. They may believe that thinking certain thoughts or doing certain behaviors can prevent a negative outcome or bring about a positive outcome. This type of thinking can lead to compulsive rituals or behaviors aimed at preventing perceived harm or ensuring a desired outcome.
Somatic Obsessions
Somatic obsessions involve intrusive thoughts or fears related to the body. People with somatic obsessions may obsess about having a serious medical condition, perceiving normal bodily sensations as something sinister, or fear of losing control over bodily functions. These obsessions can lead to excessive reassurance-seeking or avoidance of situations that trigger these thoughts.
Just Right Feelings
Some individuals with OCD may experience a compulsion to achieve a “just right” feeling. They may feel the need to touch, tap, or arrange objects until they feel a sense of completeness or satisfaction. This compulsion is driven by a need for symmetry, order, and a feeling of control.
Note: It’s important to remember that each individual with OCD experiences a unique combination of obsessions and compulsions. The severity and impact of these symptoms can vary from person to person.
In conclusion, Obsessive Compulsive Disorder is a complex mental health condition with various types of obsessions and compulsions. Understanding these different manifestations is crucial for proper diagnosis and treatment.
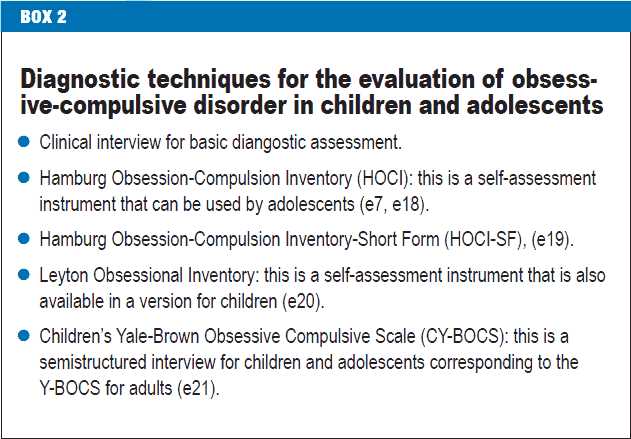
Diagnosis and Assessment of Obsessive Compulsive Disorder
Diagnosis:
Diagnosing obsessive-compulsive disorder (OCD) involves a thorough assessment of the individual’s symptoms and behaviors. Mental health professionals typically rely on both self-reported information from the individual and observations made during clinical interviews. The following criteria, based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), are used to diagnose OCD:
- Presence of obsessions, defined as recurrent and persistent thoughts, urges, or images that cause distress or anxiety.
- Compulsions, which are repetitive behaviors or mental acts performed in response to the obsessions.
- The individual recognizes that the obsessions or compulsions are excessive or unreasonable.
- The obsessions and compulsions consume a significant amount of time, typically more than an hour per day.
- The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- The symptoms are not due to the physiological effects of a substance or another medical condition.
Assessment:
Assessing OCD involves gathering comprehensive information about the individual’s mental health history, symptoms, and functioning. The following assessment methods may be used:
- Clinical interviews: Mental health professionals conduct interviews to gather information about the individual’s symptoms, their severity, and their impact on daily life. These interviews may be structured or unstructured, depending on the clinician’s preference.
- Self-report measures: Individuals may be asked to complete questionnaires or assessments that measure the severity of their OCD symptoms. These measures often include questions about obsessive thoughts, compulsive behaviors, and the distress caused by these symptoms.
- Observations: Mental health professionals observe the individual’s behavior and note any compulsions or patterns of behavior that may indicate OCD. These observations may take place during the clinical interview or in other settings.
- Collateral information: Information from family members, friends, or other individuals close to the person with OCD may be collected to gain a broader understanding of the individual’s symptoms and functioning.
- Diagnostic criteria: As mentioned above, the DSM-5 provides specific diagnostic criteria for OCD. Mental health professionals use these criteria to determine whether an individual meets the diagnosis.
Overall, the diagnosis and assessment of obsessive-compulsive disorder involve a comprehensive evaluation of the individual’s symptoms, functioning, and history. This information helps mental health professionals develop an appropriate treatment plan tailored to the specific needs of the individual.
Treatment Options for Obsessive Compulsive Disorder
Treatment for Obsessive Compulsive Disorder (OCD) typically involves a combination of medication and therapy. The specific treatment plan may vary depending on the severity of symptoms and individual needs. Here are some common treatment options for OCD:
1. Cognitive Behavioral Therapy (CBT)
CBT is a type of therapy commonly used to treat OCD. It aims to help individuals identify and change unhealthy thought patterns and behaviors. In the case of OCD, CBT typically involves exposure and response prevention (ERP) therapy. The individual is gradually exposed to their obsessions and prevented from carrying out their usual compulsions, allowing them to learn healthier coping mechanisms.
2. Medication
Medication can be an effective treatment option for OCD. Selective serotonin reuptake inhibitors (SSRIs) are the most commonly prescribed medications for OCD. These medications work by increasing the available levels of serotonin in the brain, which can help reduce obsessions and compulsions. It is important to work closely with a healthcare provider to find the right medication and dosage for each individual.
3. Deep Brain Stimulation (DBS)
Deep brain stimulation is a more invasive treatment option for severe cases of OCD. It involves surgically implanting electrodes in specific areas of the brain that are thought to be involved in the development of OCD symptoms. These electrodes deliver electrical impulses that help regulate brain activity and reduce symptoms. DBS is typically only used when other treatment options have proven ineffective.
4. Support Groups
Support groups can be a valuable resource for individuals with OCD. These groups provide a safe and supportive environment for individuals to share their experiences, learn from others, and receive emotional support. Support groups can be in-person or online and may be organized by healthcare providers, nonprofit organizations, or individuals with lived experience of OCD.
5. Lifestyle Changes
In addition to professional treatment, making certain lifestyle changes can also help manage OCD symptoms. This may include reducing stress, practicing relaxation techniques such as meditation or deep breathing exercises, getting regular exercise, and maintaining a healthy diet. These lifestyle changes can contribute to overall well-being and may complement other treatment options.
6. Family Therapy
Family therapy can be beneficial for individuals with OCD, as it involves working with family members to improve communication, understanding, and support. It can help family members learn strategies to assist their loved ones in managing their symptoms and provide a network of support in the recovery process.
It is important to remember that treatment for OCD is highly individualized, and what works for one person may not work for another. It may take time to find the right combination of treatments that effectively manage symptoms. If you or someone you know is struggling with OCD, it is essential to seek professional help for an accurate diagnosis and appropriate treatment.
Cognitive Behavioral Therapy for Obsessive Compulsive Disorder
One of the most effective treatments for Obsessive Compulsive Disorder (OCD) is Cognitive Behavioral Therapy (CBT). This form of therapy focuses on identifying and changing unhealthy patterns of thinking and behaving that contribute to the symptoms of OCD. CBT for OCD is based on the understanding that our thoughts and beliefs can influence our behavior and emotions.
CBT for OCD typically involves several components:
- Educating the individual: The therapist helps the individual understand the nature of OCD and how it affects their thoughts and behaviors. This knowledge is crucial for developing insight and motivation to change.
- Identifying triggers and obsessions: The therapist helps the individual identify the specific situations, thoughts, or objects that trigger their obsessive thoughts and compulsive behaviors. This step is essential for developing strategies to manage and overcome these triggers.
- Challenging obsessive thoughts: The therapist guides the individual in questioning the validity and rationality of their obsessive thoughts. This process involves examining evidence for and against these thoughts and developing more realistic and balanced ways of thinking.
- Developing coping strategies: The therapist works with the individual to develop healthy coping strategies to deal with the distress caused by obsessive thoughts or the urge to engage in compulsive behaviors. These strategies may include relaxation techniques, distraction techniques, or exposure and response prevention exercises.
- Gradual exposure and response prevention: This is a key component of CBT for OCD. The individual is gradually exposed to situations or objects that trigger their obsessions while refraining from engaging in the associated compulsive behaviors. Through repeated exposure and prevention of the compulsive response, the individual learns that their fears are irrational and that they can tolerate the anxiety without performing the compulsions.
- Relapse prevention: The therapist helps the individual develop a plan to prevent relapse and maintain progress after the completion of therapy. This may involve identifying potential triggers, developing strategies to cope with stress, and maintaining healthy habits and routines.
CBT for OCD is typically conducted over a series of sessions, with each session building upon the progress made in the previous session. The individual is actively involved in the therapy process and is encouraged to practice the skills learned outside of therapy sessions. CBT has been found to be highly effective in reducing the symptoms of OCD and improving overall quality of life.
In addition to CBT, medication can also be used in the treatment of OCD. In some cases, a combination of medication and therapy may be recommended for the best outcomes. It is important for individuals with OCD to work with a qualified mental health professional to determine the most appropriate treatment approach for their specific needs.
Medications for Obsessive Compulsive Disorder
Medication is an important component of the treatment plan for obsessive-compulsive disorder (OCD). While therapy, such as cognitive-behavioral therapy, is often the first-line treatment for OCD, medications can be prescribed to help manage symptoms and improve overall functioning.
There are various types of medications used to treat OCD:
- Selective Serotonin Reuptake Inhibitors (SSRIs): SSRIs are the most commonly prescribed medication for OCD. They work by increasing the availability of serotonin, a chemical in the brain that helps regulate mood and behavior. Examples of SSRIs include fluoxetine, sertraline, and fluvoxamine.
- Tricyclic Antidepressants (TCAs): TCAs are an older class of antidepressants that can also be used to treat OCD. They work by increasing the levels of serotonin and norepinephrine in the brain. Clomipramine is a TCA commonly prescribed for OCD.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): SNRIs are another class of antidepressant medications that can be used for OCD. They work by increasing the availability of both serotonin and norepinephrine in the brain. Venlafaxine is an SNRI sometimes prescribed for OCD.
- Benzodiazepines: Benzodiazepines are a type of medication that can help reduce anxiety symptoms associated with OCD. They work by slowing down the activity of the central nervous system. Examples of benzodiazepines used for OCD include clonazepam and diazepam. However, these medications are usually used as a short-term solution due to the risk of dependence.
In addition to these medications, other medications such as antipsychotics may be prescribed in some cases. Antipsychotics can help alleviate symptoms of OCD by affecting certain neurotransmitters in the brain.
It is important to note that medications should always be prescribed and monitored by a qualified healthcare professional. Different medications may have different side effects and interactions, so it’s crucial to communicate openly with your healthcare provider about any concerns or changes in symptoms.
| Pros | Cons |
|---|---|
|
|
Overall, medication can be a helpful tool in managing OCD symptoms, especially when used in conjunction with therapy. It is essential to work closely with a healthcare provider to find the most effective medication and dosage for your specific needs.
Questions and answers
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder (OCD) is a mental health disorder that is characterized by recurring and unwanted thoughts, as well as repetitive behaviors. Those with OCD often feel compelled to perform these behaviors in order to alleviate their anxiety and distress.
What are the possible causes of OCD?
The exact cause of OCD is not known, but it is believed to be a combination of genetic, neurological, and environmental factors. Some research suggests that imbalances in certain brain chemicals may play a role in the development of OCD.
What are the common symptoms of OCD?
Common symptoms of OCD include obsessive thoughts, such as fear of contamination or a need for symmetry, and compulsive behaviors, such as excessive hand washing or checking. Individuals with OCD often feel unable to control these thoughts and behaviors, which can cause significant distress and interfere with daily life.
What are the treatment options for OCD?
Treatment for OCD typically involves a combination of medication, such as selective serotonin reuptake inhibitors (SSRIs), and therapy, such as cognitive behavioral therapy (CBT). CBT can help individuals with OCD recognize and challenge their obsessive thoughts, as well as develop healthier coping strategies. In some cases, a procedure called deep brain stimulation may be used for severe, treatment-resistant OCD.